PATTERN OF DISEASE PROGRESSION FOLLOWING LOCOREGIONAL TREATMENT IN OLIGOMETASTATIC STS PATIENTS
PO-1556
Abstract
PATTERN OF DISEASE PROGRESSION FOLLOWING LOCOREGIONAL TREATMENT IN OLIGOMETASTATIC STS PATIENTS
Authors: Lucia Angelini1, Mauro Loi1, Andrea Gaetano Allegra1, Daniela Greto1, Luca Burchini1, Guido Scoccianti2, Francesco Muratori2, Domenico Andrea Campanacci2, Giuliana Roselli3, Annarita Palomba4, Carlotta Becherini1, Chiara Mattioli1, Michele Ganovelli1, Barbara Guerrieri1, Maria Grazia Carnevale1, Marianna Valzano1, Giulio Francolini1, Erika Scoccimarro1, Icro Meattini1, Beatrice Detti1, Gabriele Simontacchi1, Chiara Arilli5, Marta Casati5, Lorenzo Livi1
1AOU-Careggi, University of Florence, Radiation Oncology, Florence, Italy; 2AOU-Careggi, University of Florence, Orthopedic Oncology & Reconstructive Surgery Department, Florence, Italy; 3AOU-Careggi, University of Florence, Department of Radiology, Florence, Italy; 4AOU-Careggi, University of Florence, Pathology Department, Florence, Italy; 5AOU-Careggi, University of Florence, Medical Physics Unit, Florence, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Locoregional treatments (LT) for oligometastatic soft tissue sarcoma (STS) are increasingly being used, especially in light of the poor response to chemotherapy. However, disease control is still debated, in particular due to risk of early polymetastatic conversion. In this study we retrospectively analyzed the clinical course of oligometastatic STS after LTs.
Material and Methods
In this retrospective study, we evaluated a cohort of 19 patients with oligometastatic (i.e. ≤5 extracranial metastasis) STS, treated with stereotactic body radiotherapy (SBRT) and/or surgery from February 2014 to April 2022 for 42 metastases.
For each patient age, sex, STS site, chemotherapy prior to LT, LT type (surgery/SBRT), number of LT and the interval from diagnosis to metastatic relapse (cut-off: 24 months) were collected. Local control (LC) was defined as lack of progression of the treated site until last follow-up or death. Disease free survival (DFS) was defined as the period between the first LT and the first STS progression, last follow-up or death. Wide spread progression (WSP), corresponding to multiple site progression no longer treatable with locoregional strategies), and overall survival (OS) were calculated from date of LT to event, last follow-up, progression or death. To compare different SBRT schedule, biological effective dose (BED) was calculated assuming a α/β of 10.
Results
In our cohort, median age was 50 years (range: 39-72). Primary site was located in the limbs in 68% of patients. Adjuvant chemotherapy was administered in 70% of patients. Oligometastatic disease occurred within 24 months from diagnosis in 8 patients (42%).
All patients were treated with LT; 35% (n=6) received only surgery, 15% (n=4) only SBRT and 50% (n=9) received both. The median number of LT per patient was 2 (range: 1-6).
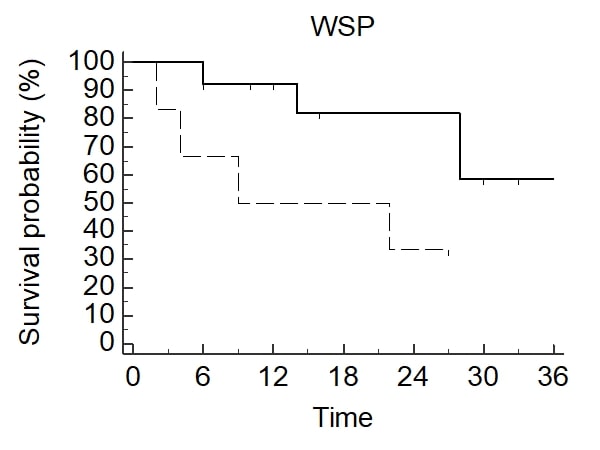
SBRT was performed in 3-5 fractions to a total dose of 30-60 Gy; median BED10 was 105 Gy (35.7-151.2). LC rate was 80% at 1 year and 72% at 2 years (Figure 1a), median not reached, with no differences between surgery and SBRT for LC (Figure 1b). No >G2 toxicities were observed in all treatments. Median DFS, WSP and OS were respectively 12 months (95% CI 3-19), 28 months (95% CI 22-53) and 35 months (95% CI 26-35). At the univariate analysis, no significant differences in LC, DFS and OS were found, according to age, sex, histology, site of STS, chemotherapy, number of LT and interval from diagnosis to metastatic relapse. A longer delay to WSP was observed in patients who experienced first metastatic recurrence ≥24 months from diagnosis (median: 9 vs 53 months, p= 0.031, HR 0.30 [0.05-1.6]) (Figure 2).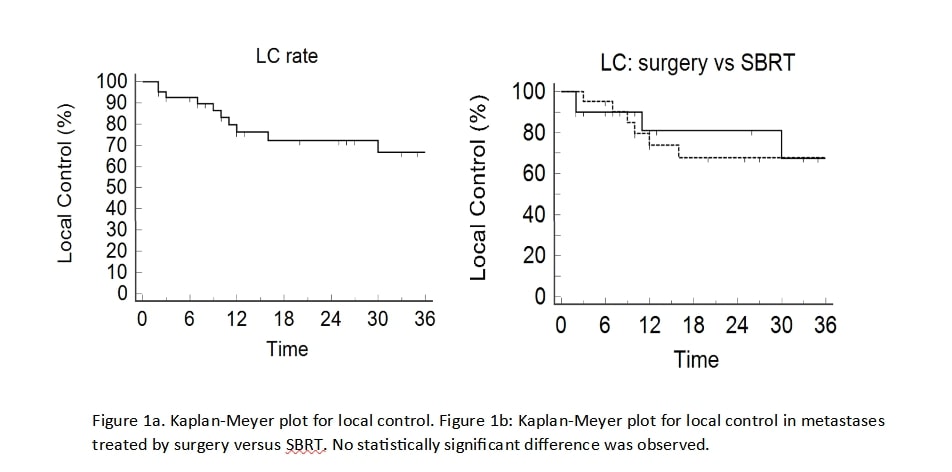
Conclusion
Oligometastatic STS patients treated with LTs experience a satisfying LC rate, without significant differences between SBRT or surgery, long progression-free interval and promising OS. Polymetastatic conversion is a late event, in particular in patients with a long interval from primary diagnosis to first metastatic relapse. Repeated LTs could be administered to extend disease control.