Patient-reported outcome measures after salvage radiotherapy for prostate cancer
Christine Vestergaard Madsen,
Denmark
PO-1462
Abstract
Patient-reported outcome measures after salvage radiotherapy for prostate cancer
Authors: Christine Vestergaard Madsen1, Martin Berg2, Ahmed Zedan1, Bjarke Mortensen2, Terje Andersen2, Henrik Nissen2, Lone Volmer1, Mette Svenson1, Tina Siersbæk1, Lars Fokdal1
1Vejle Hospital, University Hospital of Southern Denmark, Department of Oncology, Vejle, Denmark; 2Vejle Hospital, University Hospital of Southern Denmark, Radiotherapy Research Team, Department of Oncology, Vejle, Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
Salvage radiotherapy (SRT) with bicalutamide is a recommended treatment option for patients with biochemical relapse after radical prostatectomy for prostate cancer (PCa). However, early and late toxicity for both gastro-intestinal (GI) and for genito-urinary (GU) tract can be expected, making the timing for SRT still debatable.
Data on quality of life from a patient perspective are important because they enable the healthcare personnel to focus on what really matters to the patient. So far, this clinical information seems to be less investigated in patients receiving SRT and bicalutamide.
Material and Methods
Between December 2017 and June 2022, eighty-one consecutively selected patients treated with SRT (70 Gy in 35 fxt, VMAT technique) and two years of concomitant bicalutamide were included in an open prospective observational study. Systematic collection of common terminology criteria for adverse events (CTCAE v 4.0) and patient-reported outcome measures (PROMs) were done at baseline (BL), at end of SRT treatment (EOT), and at regular intervals during a five-year follow-up (4 w, 3 m, 6 m, 9 m, 12 m, 18 m, 24 m, 30 m, 36 m, 48 m, 60 m).
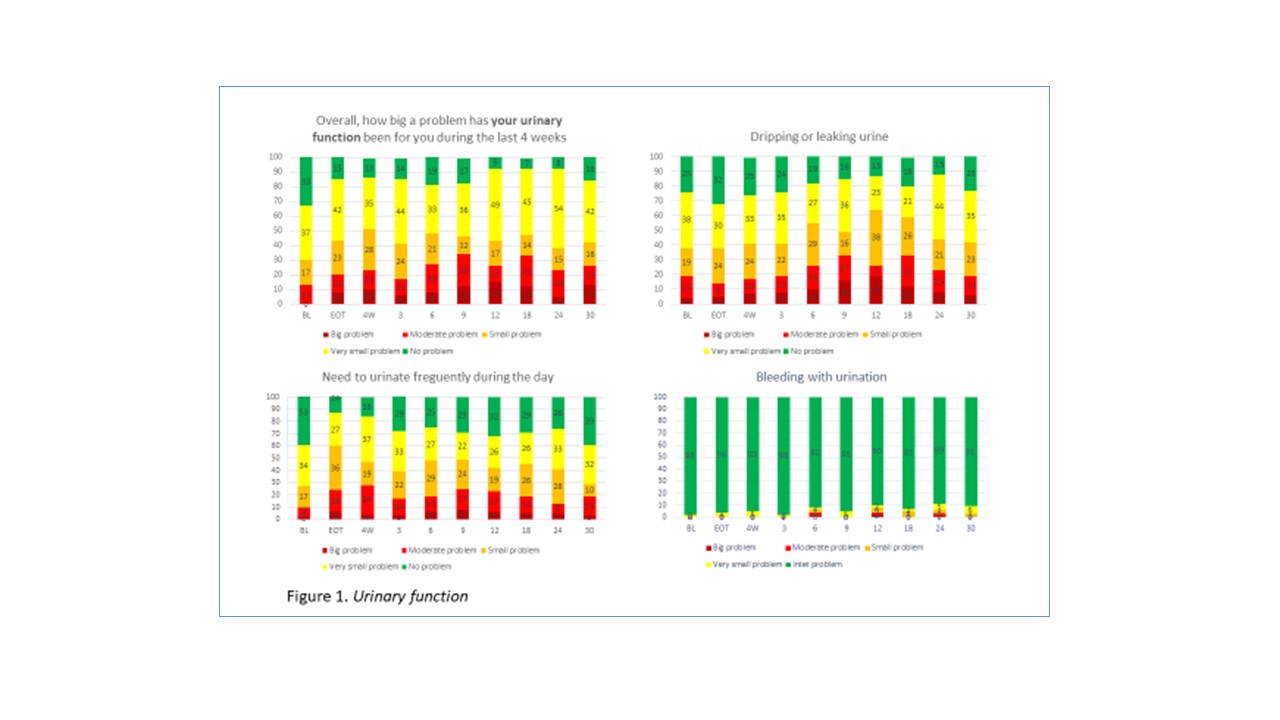
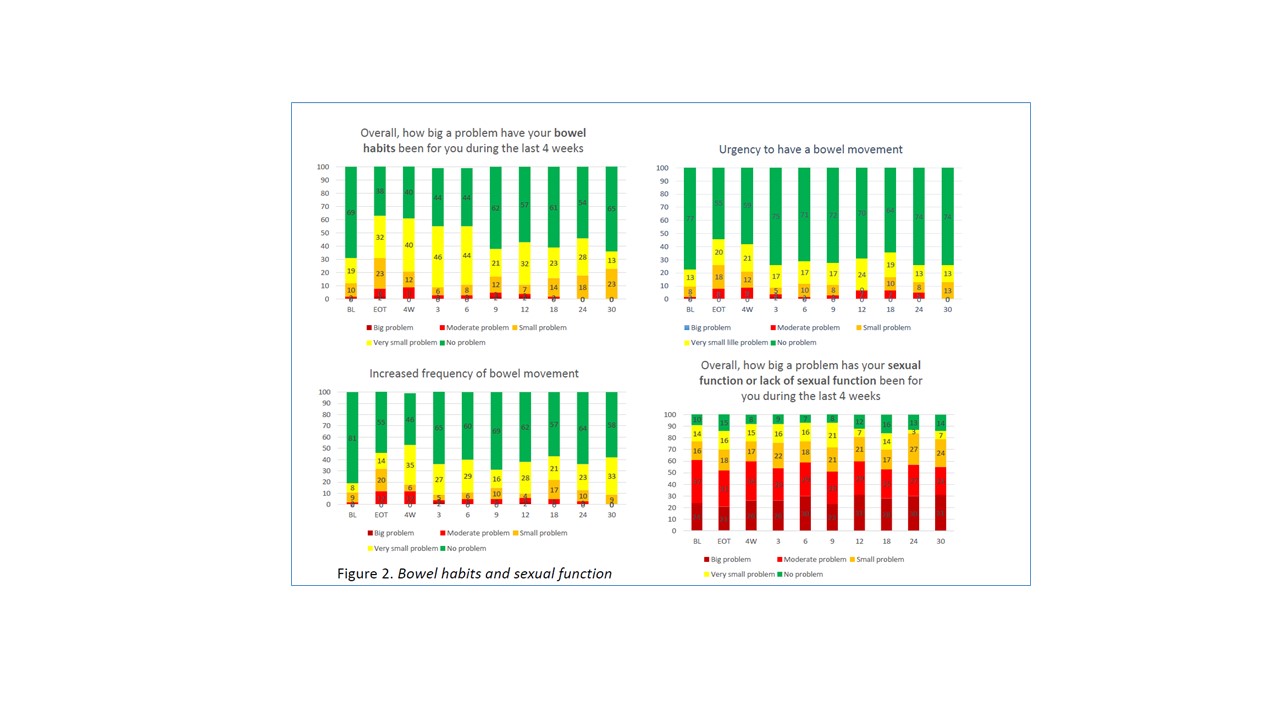
EPIC-26, EORTC QLQ-C30, and supplementary questions from QLQ-PR25 were used for PROMs assessing health-related quality of life. In this study results on urinary function, bowel habits, and sexual function are presented.
Results
The median follow-up was 23 (range 2 - 50) months and 93% of the patients received two years of bicalutamide. At BL, the median PSA was 0.2 (range <0.1- 4.1), the median age was 68 (range 50 - 75) years, and the median body mass index (BMI) was 27.5 (range 21.6 - 37.2). Charlson Comorbidity Index score >1 was found in 31.6% of the patients and 21% were still active smokers.
The prevalence rate (PR) of problems with urinary function increased at EOT (p=0.044) and after 12 months of follow-up (p=0.029). In 13% of the patients a “moderate or big problem” was reported at BL, peaking at 34% nine months after EOT, and decreasing to 26% after one year. The PR of bleeding with urination were low (figure 1).
The PR for bowel habit problems increased significantly at EOT (p=0.004) but after one year, there were no statistically significant differences in the parameters (p=0.776). The PR of a “moderate or big problem”, was 2% at BL, 8% at EOT, peaking at 9% four weeks after EOT (figure 2).
Sixty percent reported a “moderate or big problem” regarding sexual dissatisfaction at BL, and PR showed only minor variations throughout the follow-up period (p=0.317 after one year) (figure 2).
Conclusion
A subset of PCa patients receiving SRT with concomitant bicalutamide will experience changes in bowel habits and urinary function resulting in “moderate to big problems”. Furthermore, a considerable number of patients will experience sexual dissatisfaction, but without significant relation to SRT. These observations could be used to improve patients’ involvement in shared decision-making as well as rehabilitation after SRT.