MR Delta Radiomics during Radiotherapy to Prostate Cancer: Does Dose per Fraction Matter?
Martin Swinton,
United Kingdom
PO-1460
Abstract
MR Delta Radiomics during Radiotherapy to Prostate Cancer: Does Dose per Fraction Matter?
Authors: Martin Swinton1, Robin Portner2, Leah Brooks3, Jim Zhong4, Cynthia Eccles5, Gareth Price6, Andy Hudson1, Robert Bristow7, Alan McWilliam7, Ananya Choudhury1, Peter Hoskin1
1Christie Hospital, Clinical Oncology, Manchester, United Kingdom; 2Rosemere Cancer Centre, Clinical Oncology, Preston, United Kingdom; 3University of Manchester, Medicine, Manchester, United Kingdom; 4University of Leeds, Radiology, Leeds, United Kingdom; 5Christie Hospital, Radiotherapy, Manchester, United Kingdom; 6University of Manchester, Cancer Digital Sciences and Machine Learning, Manchester, United Kingdom; 7University of Manchester, Cancer Sciences, Manchester, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Developing imaging biomarkers in prostate cancer (PCa) that associate with response to radiotherapy (RT) or Androgen Deprivation Therapy (ADT) may identify patients for radiation boost or additional adjuvant therapy. MR images acquired during prostate RT on an MR Linac allows analysis of dynamic changes in image features during treatment. We aimed to characterise changes in prostate radiomic features before and after ADT and during RT in PCa patients receiving either hypofractionated (60 Gy in 20# over 4 weeks) or stereotactic ablative radiotherapy (SABR – 36.25Gy in 5# over 2 weeks).
Material and Methods
This is a retrospective radiomic analysis of 20 men receiving RT to their prostate on an MR Linac after neoadjuvant ADT. T2-weighted images acquired on a 1.5T Elekta Unity MR Linac were analysed on each treatment day R0-R4 for those receiving 5#. For 20#, imaging was acquired from Day 1 (R0) and at the end of each week of treatment (R1-R4). Regions of Interest of dominant intraprostatic lesion (DIL) and whole prostate (WP) were outlined on R0 and a co-registration method used to copy contours to R1-R4. A diagnostic MRI acquired prior to ADT (D0) was also analysed. MR images across treatment for each patient were normalised to the first fraction. First order radiomic features for WP and DIL extracted following the imaging standardisation biomarker initiative guidelines. Mean and median intensity, kurtosis, uniformity and entropy were extracted, and Mann-Whitney U testing assessed differences between fractionations
Results
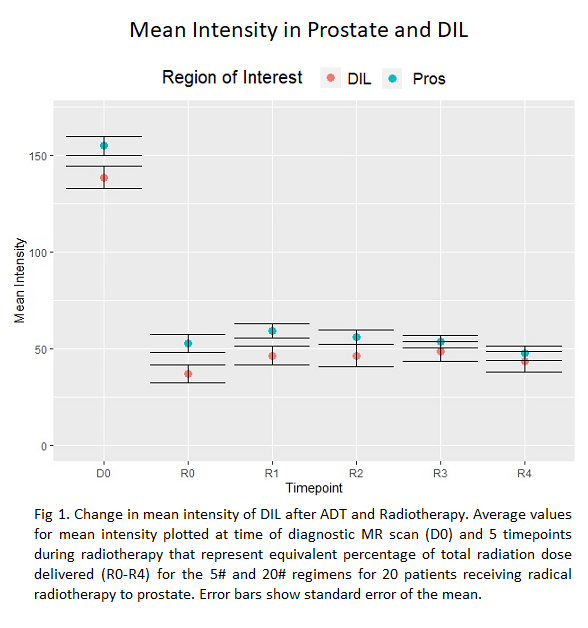
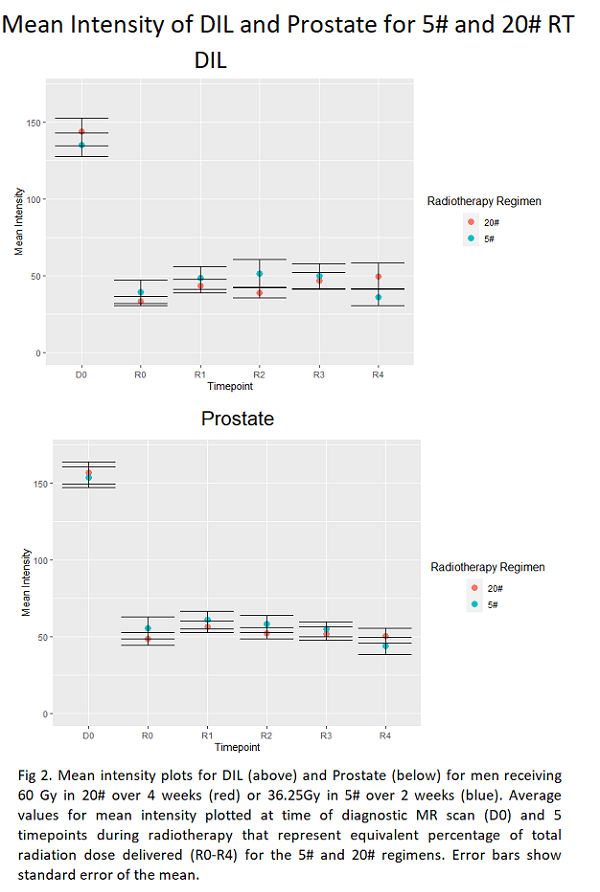
8 men received 20# and 12 men received 5# RT. Mean Intensity in both WP and DIL reduced between D0 and R0 (Fig. 1). Mean Intensity in WP was greater than DIL at D0 (p=0.04) and R0 (p<0.01) but converged during RT with no difference at R3 (p=0.13) or R4 (p=0.32). An increase in mean intensity from R0 to R1 followed by a reduction by R5 was seen in both DIL and WP (Fig. 1). Mean intensity curves for both WP and DIL did not differ for 20# and 5# regimens (Fig. 2). Compared to WP, DIL had lower entropy and higher uniformity at D0 with differences reducing at later time points (R0-R4). Kurtosis showed no difference between WP and DIL at D0 but separated with higher values in WP than DIL after ADT and RT.
Conclusion
Analysed radiomic features – excepting kurtosis - showed convergence of values for WP and DIL over time, implying these regions become less distinct with treatment. The early rise and fall in mean intensity during RT implies an imaging biomarker for treatment response should be acquired at multiple time points during treatment to fully understand dynamic changes during RT. The treatment time of the 5# regimen is half the 20# regimen, however when images are sampled at points with equivalent percentage of total dose received, the 5 and 20# curves show no difference in mean intensity suggesting biological processes underly MR imaging changes occur at an earlier time points with higher doses per fraction.