Concordance of number and site of metastases with PET/CT vs conventional imaging in prostate cancer
HODA ABDEL-ATY,
United Kingdom
PO-1457
Abstract
Concordance of number and site of metastases with PET/CT vs conventional imaging in prostate cancer
Authors: Hoda Abdel-Aty1, Nabil Hujairi2, Iain Murray2, Nicholas van As1, Nicholas James1
1Institute of Cancer Research. The Royal Marsden NHS Foundation Trust, Radiotherapy and Imaging, London, United Kingdom; 2The Royal Marsden NHS Foundation Trust, Radiology and Nuclear medicine, London, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
PET/CT is more accurate than conventional imaging for staging prostate cancer. Limited data exists on PET/CT directed clinical outcomes. We aim to determine the per-patient concordance of PET/CT with conventional imaging based on the number and site of metastatic lesions, and explore the patterns of PET/CT directed treatment in newly diagnosed metastatic prostate cancer.
Material and Methods
245 patients with PET/CT detected newly diagnosed metastatic prostate cancer were retrospectively reviewed. Patients with baseline PET/CT and bone scintigraphy were included. Images from baseline PET/CT and conventional imaging (low dose CT of PET and bone scintigraphy) were reviewed. Patients were sub-grouped into oligometastatic disease (OMD) and polymetastatic disease (PMD). OMD was defined as ≤5 bone and/or non-regional nodal metastases. Subgroup concordance was the same sub-group assigned for each modality.
Results
Between 2015 and 2021, 74/245 (30%) patients were analysed. 54/74 (73%), 9/74 (12%) and 11/74 (15%) patients had 68Ga PSMA-11, 18F PSMA-1007 and 18F-Choline PET/CT respectively. 50/74 (68%) patients had ISUP grade group 5, and 70/74 (95%) patients had ≥T3 disease. Median age was 69 (range 48-86) years. Concordance for number of bone, nodal and visceral metastases is summarised in figure 1.
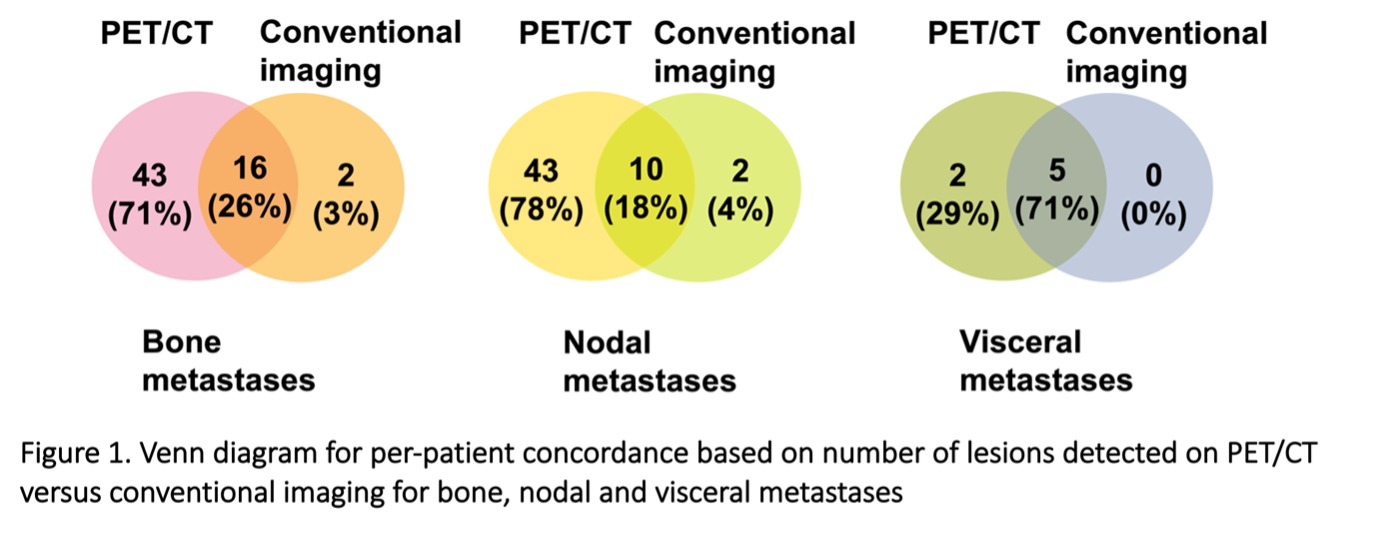
The total number of metastases detected with PET/CT was increased by 3-fold for bone metastases, and 2-fold for nodal metastases.
43/74 (58%) had bone metastases on bone scintigraphy, concordance for site was present in 39/43 (91%) patients. 35/74 (47%) patients had nodal metastases on conventional imaging, concordance for site was present in 33/35 (94%) patients.
38/74 (51%) patients were PET-OMD and 35/74 (47%) were PET-PMD, with a median PSA of 33 (range 3.2-400) ng/mL, and 61 (range 4.8-5400) ng/mL respectively. Concordance for OMD is summarised in figure 2.
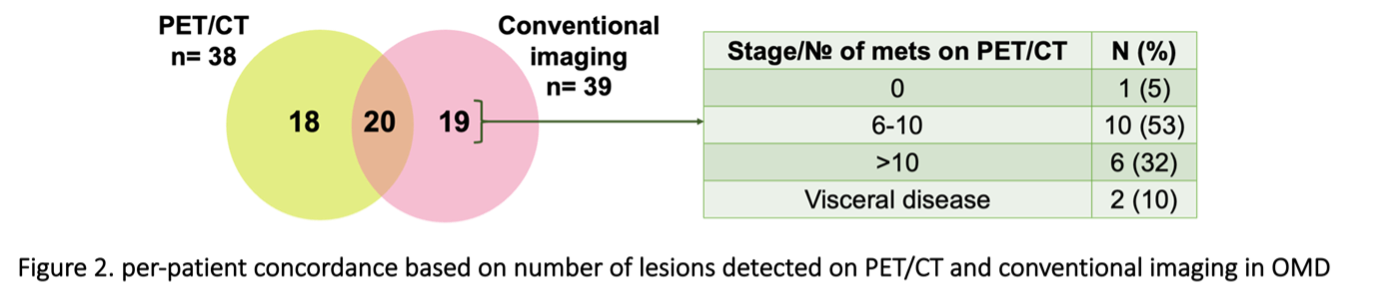
In PET-PMD, 16/35 (46%) had 6-10 lesions and 12/35 (34%) had >10 lesions. In patients with 6-10 lesions, 10/16 (62) were OMD, and 5/16 (31%) were M0 on conventional imaging. In patients with > 10 lesions, 2/12 (17%) were PMD, 6/12 (50%) were OMD, and 4/12 (33%) were M0 on conventional imaging.
27/38 (71%) PET-OMD patients had prostate radiotherapy (± pelvic nodes, ± bone metastases). 18/35 (51%) PET-PMD patients had prostate radiotherapy (± pelvic nodes, ± bone metastases), all of which were “low-volume” on conventional imaging as per CHAARTED criteria.
Conclusion
PET/CT detects more metastases than conventional imaging. The magnitude of effect with a “right stage shift” poses implications on treatment decisions in the metastatic setting with potential overtreatment or undertreatment of patients. Work is on-going to expand the patient dataset to determine the patterns of response and relapse following PET/CT-directed treatment.