Using weekly digital patient-reported outcomes to evaluate toxicity for patients at the MR-linac
PO-1536
Abstract
Using weekly digital patient-reported outcomes to evaluate toxicity for patients at the MR-linac
Authors: Pia Krause Moeller1, Uffe Bernchou2, Tine Schytte1, Helle Pappot3, Anders Smedegaard Bertelsen2, Lars Dysager4, Christina Junker Nyborg1, Karin Brochstedt Dieperink5
1Odense University Hospital, Department of Oncology, Odense, Denmark; 2Odense University Hospital, Laboratory of Radiation Physics, Odense, Denmark; 3Rigshospitalet, University Hospital of Copenhagen, Department of Oncology , Copenhagen, Denmark; 4Odense Universitets Hospital, Department of Oncology, Odense, Denmark; 5Odense University Hospital, Department of Oncology, Odense , Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
Toxicity monitoring of frequent longitudinal patient-reported outcomes (PROs) ensures timely detection of changes in symptomatic adverse events (AEs). However, since treatment with online MR-guided radiotherapy (MRgRT) was introduced, no studies have prospectively collected and monitored weekly changes in PROs over time. Therefore, we aimed to investigate a clinical relevant worsening in urinary frequency, acute AE trajectories, time to first peak of AEs and symptom persistence for patients with prostate cancer (PCa) treated with online MRgRT.
Material and Methods
Patients with PCa referred for MRgRT at the 1.5 T Unity MR-linac from November 2020 – May 2022 were eligible for enrollment. Patients reported digital PROs (ePROs) weekly from baseline until four weeks following MRgRT and at follow-up weeks eight and 12. A systematically developed pelvic item set with 18 AEs was used for ePRO collection, including a free-text AE response option. Clinicians had access to real-time monitoring of the patients using ePROs filed directly in the medical records. The primary endpoint was defined as a clinically relevant two-level increase in urinary frequency for more than one week.
Results
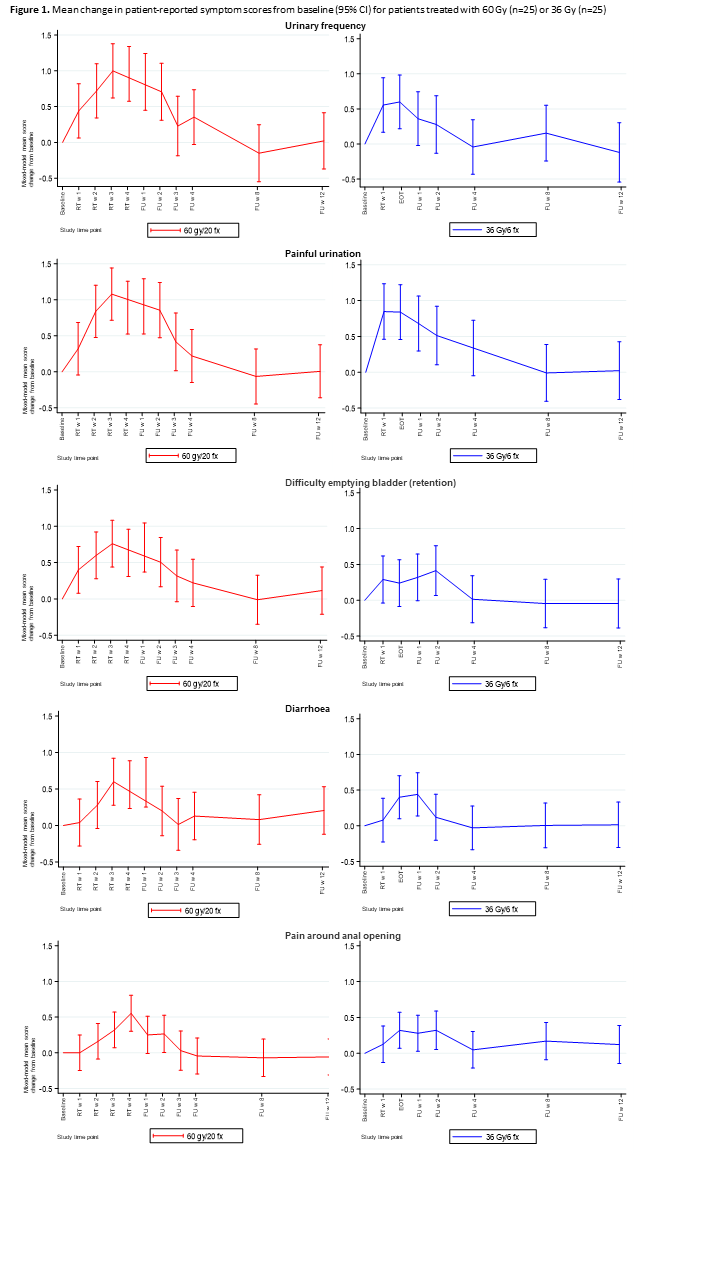
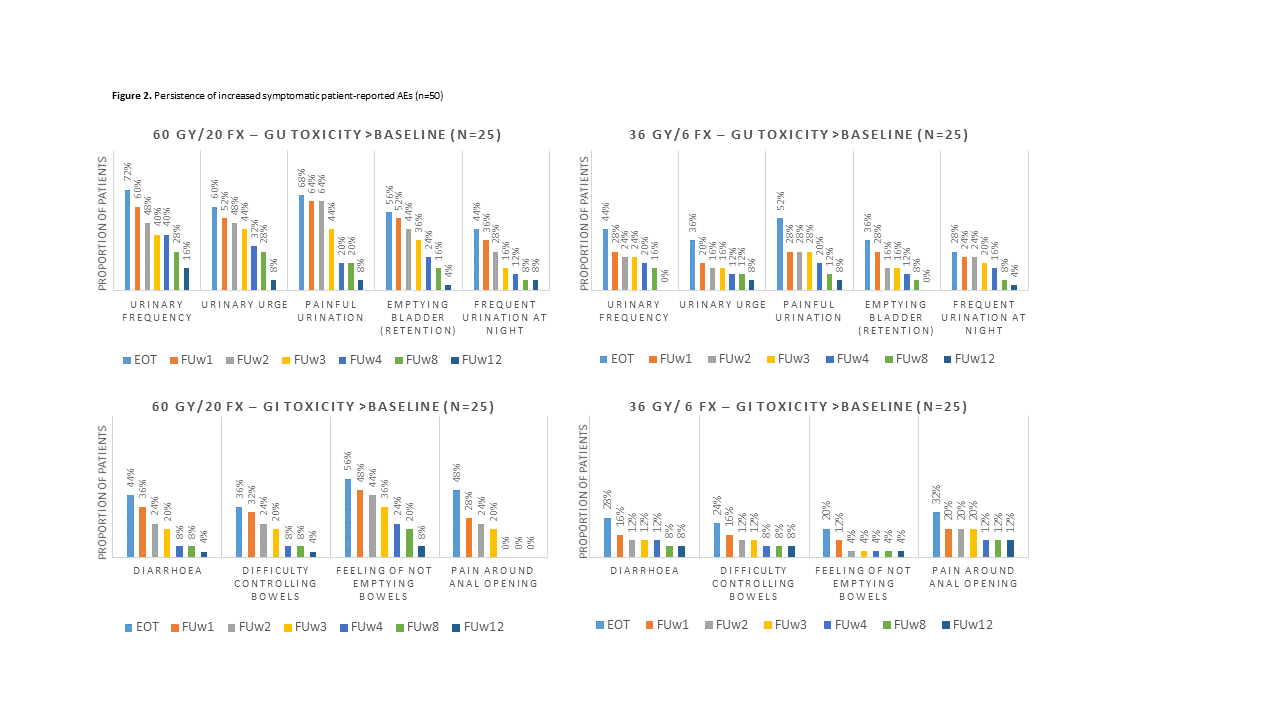
Fifty patients with PCa were included in the analyses; 25 had localised PCa treated with 60 Gy/20 Fx (5 Fx/week), and 25 had low-volume metastatic PCa treated with 36 Gy/6 Fx (2-3 Fx/week). The median age was 71 (60-81), and 92% completed ePROs (8% on paper). The mean adherence rate to weekly ePRO was 94%. A clinically relevant increase in urinary frequency was reported by 20% of patients (28% (60 Gy), 12% (36 Gy)). Figure 1 shows selected AE trajectories. The 60Gy cohort revealed the highest significant mean changes in AE scores in the third week of MRgRT. In the 36 Gy cohort, the urinary irritative AEs peaked during MRgRT, but urinary obstructive AEs, diarrhoea and rectal pain peaked during follow-up weeks 1-2. Overall, the median time to the patients’ first peak of the AEs was two weeks for the 60 Gy cohort and one week for 36 Gy. Twelve weeks following treatment, the most persistent symptom in the 60 Gy cohort was increased urinary frequency (16%); for the 36 Gy cohort, increased pain around the anal opening persisted (12%) (Figure 2). Additional AEs were reported at all times by 32% of patients, with 14% having severe or very severe symptoms.
Conclusion
This is the first study to explore acute AE trajectories for PCa patients receiving online MRgRT. A clinically relevant increase in urinary frequency was found for one-fifth of patients. The mean changes in AEs for the two cohorts peaked at different time points. Twelve weeks after MRgRT, increased urinary frequency and rectal pain persisted as the most common symptom for the 60 Gy and 36 Gy cohort, respectively. One-third of the patients reported additional symptoms potentially treatment-related. To optimise future MRgRT regimes and supportive care, toxicity monitoring of weekly ePROs ensures timely detection of changes in patient-perceived AEs.