SBRT boost is a viable alternative to HDR brachytherapy boost for prostate cancer patients
PO-1524
Abstract
SBRT boost is a viable alternative to HDR brachytherapy boost for prostate cancer patients
Authors: Daša Grabec1, Aleš Majdič1, Janka Čarman1, Borut Kragelj1
1Institute of Oncology Ljubljana, Radiotherapy, Ljubljana, Slovenia
Show Affiliations
Hide Affiliations
Purpose or Objective
The combination of 50.4Gy/28fx external beam radiotherapy (EBRT) and high dose rate brachytherapy (HDRB) boost with median prostate dose D90% of 19Gy/3fx resulted in PET/CT defined local failure incidence rate of 3/88 patients with the median follow up of 8 years.
We hypothesise that similar efficiency is expected with stereotactic body radiotherapy (SBRT) boost. Here we develop the SBRT boost protocol focusing on the prevention of urethral toxicity, while escalating the dose on the dominant intraprostatic lesion.
Material and Methods
Treatment plans for SBRT boost were constructed to meet the prescribed dose presented in table I, where GTVp is dominant intraprostatic lesion, CTVp is prostate and PTVp is prostate with margin. Urethra was defined with the fusion of urethra and sphincter urethrae membranaceae. For SBRT 2 mm expansion was used to define PRV. Dose to the urethra (HDRB) or urethra PRV (SBRT) was limited with Dmax < 110% for HDRB and D1% < 105% for SBRT. We retrospectively compared the dose distributions of HDRB and of SBRT boost plans for 10 patients.
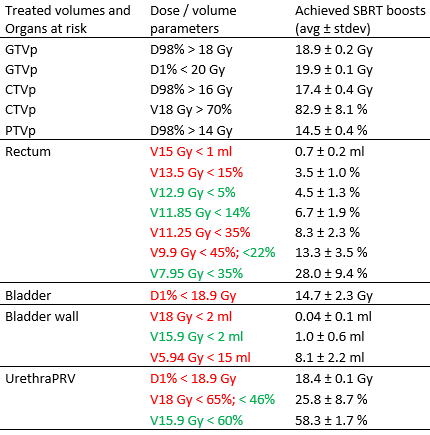
Table I: Dose constraints for the SBRT boost planning and average achieved values for 10 SBRT boost plans. Dose constraints in red are obligatory and in green are optional.
Results
The average maximal dose (D1%) to urethra was 18.4 ± 0.1 Gy in SBRT boost vs 19.4 ± 0.1 Gy in HDRB boost. Average V18 Gy was 25.8 ± 8.7 % in SBRT boost vs 43.9 ± 13.2 % in HDRB boost and average V15.9 Gy was 58.3 ± 1.7 % in SBRT boost vs 62.4 ± 15.3 % in HDRB boost.
The example of HDRB and SBRT boost doses are shown in Figure 1. The main limiting constraint in SBRT is dose on the urethra. On the contrary to brachytherapy where urethra is fixed, in SBRT urethra PRV has to be defined even though prostate is tracked with fiducial markers.
Few patients are already being treated according to the presented protocol.
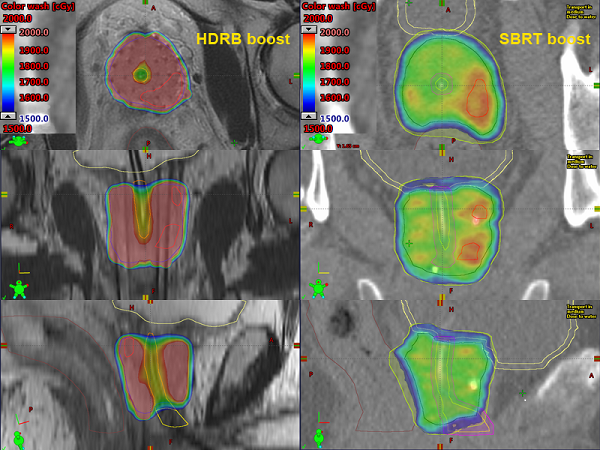
Fig 1: Example of HDRB and SBRT dose distributions
Conclusion
We demonstrated that it is possible to achieve SBRT boost plans of escalated dose to the dominant intraprostatic lesion while maintaining acceptable urethral dose. This technique is suitable for patients that undergo EBRT but due to medical conditions (long COVID, acute myocardial infarction…) cannot receive scheduled HDRB boost. When prior to EBRT is known that patient is not suitable for brachytherapy, other regimes of external irradiation (60Gy/20fx, 42.7Gy/7fx) are used.