Ga68-PSMA PETCT response-adapted metastasis directed RT in hormone-sensitive prostate cancer
PO-1521
Abstract
Ga68-PSMA PETCT response-adapted metastasis directed RT in hormone-sensitive prostate cancer
Authors: Prachi Mehta1, Ajay Thomas1, Ashish Mohite2, Varun Ramchandani2, Priyamvada Maitre1, Archi Agarwal2, Venkatesh Rangarajan2, Vedang Murthy1
1TMC, Radiation Oncology, Mumbai, India; 2TMC, Nuclear Medicine, Mumbai, India
Show Affiliations
Hide Affiliations
Purpose or Objective
The role of metastasis-directed radiotherapy (MDT) in hormone-sensitive prostate cancer is being explored actively. We report on an approach of utilising Ga68-PSMA PET-CT response to ADT for selecting patients for adding metastasis-directed RT (MDT) in node-positive and oligometastatic prostate cancer.
Material and Methods
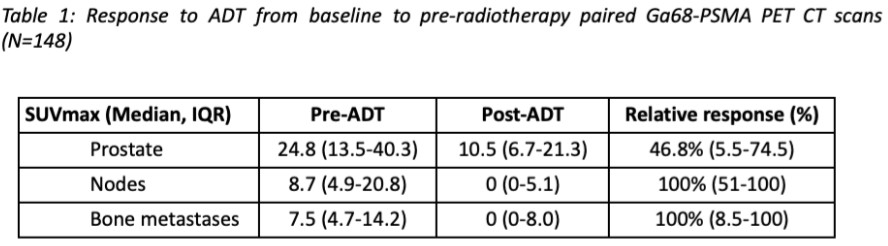
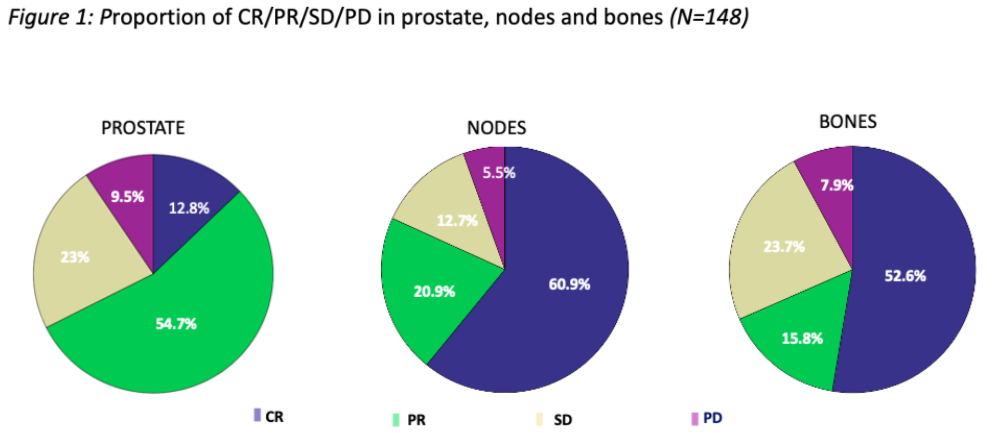
In this IRB-approved study, patients diagnosed with prostate adenocarcinoma with metastases to pelvic nodes or oligometastases, as seen on baseline staging Ga68-PSMA PETCT, were identified. All patients received long-term ADT and image-guided conformal RT to the prostate. Eligible patients had a second Ga68-PSMA PETCT scan after 4-6 months of ADT prior to RT. MDT was added only to the metabolically active residual metastases on the second scan. Change in maximum standardised uptake value (SUVmax) was estimated for prostate, nodes, and bone metastases from the baseline to pre-RT Ga68-PSMA PETCT scans. Response to ADT was categorised as complete/partial/stable/progression (CR/PR/SD/PD) using EAU-EANM consensus criteria.
Results
Total 148 patients (N1M0 = 65, M1a = 44, M1b = 39) with paired Ga68-PSMA PETCT scans were eligible and analysed, with median 6 months ADT (IQR 5-6) between the scans. 90% of patients received ADT alone without systemic intensification. Median relative decline in SUVmax was 47% (IQR 5-72) for prostate, 100% (51-100) for nodes, and 100% (8-100) for bone metastases (Table 1). The proportion of CR/PR/SD/PD in prostate, nodes, and bones is shown in figure 1. Using this PSMA PETCT response-adapted approach, 23/148 (15.5%) patients needed MDT to metabolically active residual lesions. With a median follow-up of 38 months, 26/148 (17.6%) patients developed castration-resistant prostate cancer (CRPC).
Conclusion
Ga68-PSMA PETCT-based response assessment in HSPC showed nodal and bone metastases responding better to ADT than primary prostate. Only a small proportion of patients with metabolically active residual metastases required MDT. This approach of selective risk-adapted MDT needs to be explored and validated prospectively.