Acute toxicity rates and predictors in extreme hypofractionation for localized prostate cancer
Giuseppe Carlo Iorio,
Italy
PO-1496
Abstract
Acute toxicity rates and predictors in extreme hypofractionation for localized prostate cancer
Authors: Giuseppe Carlo Iorio1, Diego Bongiovanni1, Ilaria Bonavero1, Giuliana Petruzzellis1, Sara Bartoncini1, Elena Gallio2, Valeria Chiofalo1, Erica Maria Cuffini1, Cristiano Grossi1, Mario Levis1, Umberto Ricardi1
1University of Turin, Department of Oncology, Turin, Italy; 2University of Turin, Department of Medical Physics, Turin, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
extreme hypofractionation is gradually becoming a mainstay of treatment for prostate cancer (PCa). Patients’ (pts) tolerance to such RT regimes is undoubtedly under the spotlight. Herein, we report acute toxicity data and predictors in a single-center observational analysis.
Material and Methods
this toxicity analysis pertains to a consecutive series of low-to-high-risk PCa pts treated with (LINAC-based VMAT) extreme-hypofractionation (42.7Gy/7 non-consecutive fractions-frs, 15-19 days) +/- ADT. Genitourinary (GU) and gastrointestinal (GI) acute toxicities were scored according to RTOG during the following timepoints: each RT fr, 1- and 3-months (mos) from RT end. Patient (risk-group, previous TURP, prostate cc ≤ or > 80cc, IPSS score ≤ or > 12), treatment (neoadjuvant-concomitant-adjuvant ADT use, overall treatment time-OTT ≤17 or >17 days) and dosimetric (V37Gy bladder ≤10cc, ≤15cc, ≤20cc, >20cc) variables were analyzed (logistic regression analysis) to investigate potential acute RTOG GU G2+ toxicity predictive/protective factors.
Results
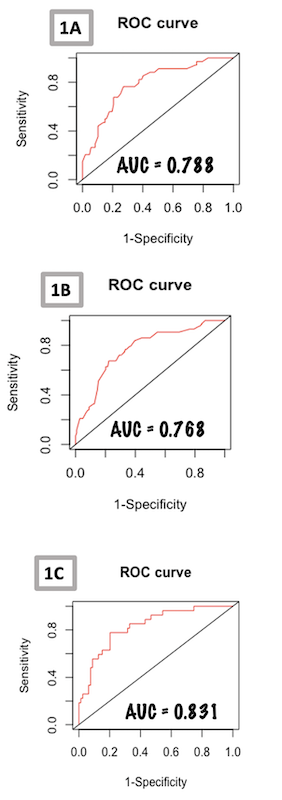
187 pts (mean age 74.5 years) were treated between May 2020 and October 2021. Most pts were classified as intermediated-risk (77.5%), followed by high-risk (18.2%) and low-risk (4.3%). ADT was administered to 56.1%. Baseline IPSS >12 was observed in 23.9%. Most pts had a prostate volume<80cc (83.9%). Previous TURP was reported for 38 pts, mainly more than 2 years before RT (31 pts). The most commonly recorded V37Gy bladder metric was 16-20cc(57.2%), followed by 11-15cc(21.4%), 0-10cc(12.3%) and >20cc(9.1%). Treatment was completed within 17 days for 66 pts, in >17 days for 121 pts. Acute RTOG GU G2+ events were observed in 23% of pts, peaking at the last fr(19.8%, 37 pts). 3 pts experiencing G2+ during the first 6 frs had <G2 at RT end. RTOG GU G2+ rate at 1-mo was 3.2% (with 2/6 experiencing G2+ for the first time) and 1.07% at 3-mos (2 pts, with 1 experiencing G2+ for the first time). Considering the 146 pts with IPSS data available at baseline, from the logistic regression analysis ADT emerged as a statistically significant GU G2+ protective factor (p<0.001; fig.1A).Excluding IPSS (due to 41 pts with missing baseline data), prostate volume>80cc resulted a statistically significant predictor(p=0.018), ADT a statistically significant protective factor (p<0.001), and the OTT>17 days a borderline significant protective factor (p=0.05; fig.1B).When employing continuous values for prostate volume cc, bladder V37Gy cc, and IPSS scores, ADT was significantly protective(p=0.001),while greater prostate volumes and higher IPSS scores resulted as significant predictors(p=0.01 and p=0.02, respectively)(fig.1C).RTOG GI G2+ rate at RT end was 2.1%, 1.07% at 1-mo, while no G2+ was recorded at 3-mos.
Conclusion
extreme hypofractionation was well tolerated, with acute GU G2+ toxicity peaking at RT end and almost disappearing at 3-mos. Larger prostates and high IPSS scores resulted as GU G2+ predictors, while ADT as the main protective factor. GI G2+ was negligible.