Prostate cancer nodal relapse: impact of CRPC and previous RT on salvage ENRT+PET guided SIB outcome
PO-1490
Abstract
Prostate cancer nodal relapse: impact of CRPC and previous RT on salvage ENRT+PET guided SIB outcome
Authors: Andrei Fodor1, Chiara Deantoni1, Laura Giannini1, Federica Ferrario1, Stefano Villa1, Paola Mangili2, Lucia Perna2, Sara Broggi2, Italo Dell'Oca1, Flavia Zerbetto3, Chiara Chissotti1, Martina Midulla1, Miriam Torrisi1, Barbara Longobardi2, Roberta Castriconi2, Antonella Del Vecchio2, Cesare Cozzarini1, Claudio Fiorino2, Nadia Di Muzio4
1IRCCS San Raffaele Scientific Institute, Department of Radiation Oncology, Milan, Italy; 2IRCCS San Raffaele Scientific Institute, Medical Physics, Milan, Italy; 3IRCSS San Raffaele Scientific Institute, Department of Radiation Oncology, Milan, Italy; 4IRCCS San Raffaele Scientific Institute & Vita-Salute San Raffaele University, Department of Radiation Oncology, Milan, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Patients treated for lymph-nodal metastases (LNM) of prostate cancer (PC) are often an inhomogeneous population, including either hormonal-sensitive (HSPC) or castration-resistant patients (CRPC), at the first or second radiation therapy (already treated with adjuvant or salvage radiotherapy, ART/SRT), who could have different prognoses. Here we report long-term outcomes of our cohort of patients treated with salvage extensive–nodal radiotherapy (ENRT) and positron emission tomography (PET)-guided simultaneous integrated boost (SIB) on PET positive LNM, considering these differences.
Material and Methods
From 02/2005 to 11/2021, >200 PC patients were treated for LNM with ENRT at a median total dose (TD)= 51.8 Gy/28 fr, and PET-guided SIB on PET+ LNM to a median TD= 65.5 Gy. For 190 patients the primary treatment was surgery, and 108 of them had already been treated with ART/SRT, before the salvage treatment for nodal relapse. Median age at relapse was 71.3 (50.7-83.9) years. Median PSA was 1.97 (0.18-187.0) ng/ml. Median number of PET+ LNM was 2 (1-20). Androgen Deprivation Therapy was prescribed for 143 patients, for a median of 25.8 months, and 46 were CRPC
Results
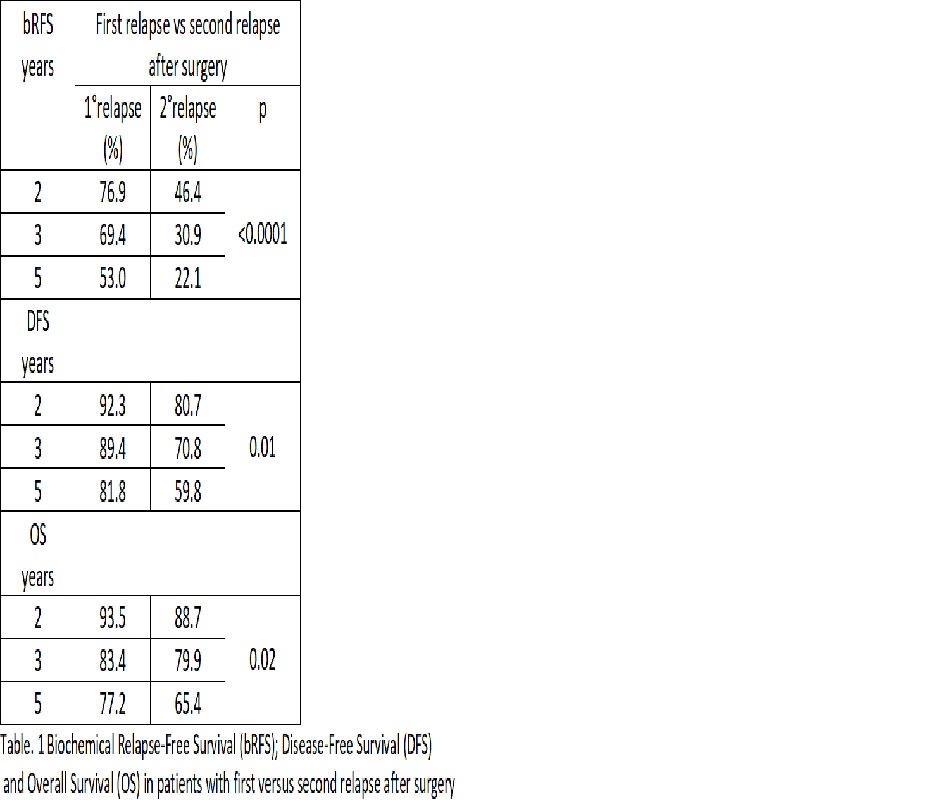
With a median follow up of 60.9 (4.1-171.2) months, actuarial median biochemical relapse-free survival (bRFS) for HSPC patients was 47.3 months vs 13.6 months for CRPC. Median disease-free survival (DFS) was 136.3 vs 65.3 months, and median overall survival (OS) 137.6 vs 60.1 months. Two-, three- and five-year Kaplan Meyer estimates of biochemical relapse-free (bRFS), disease-free (DFS) and overall survival (OS) in HSPC vs CRPC are presented in Table 1. In patients without previous RT(at first LNM relapse) vs patients with previous ART/SRT (second relapse) actuarial median bRFS was 70.2 vs 20.3 months, median DFS was not reached for patients at first relapse vs 91.7 months for second relapse, and for OS, again, median OS was not reached for patients at first relapse vs 91.7 months for second relapse. Two-, three- and five-year Kaplan Meyer estimates of biochemical relapse-free (bRFS), disease-free (DFS) and overall survival (OS) for patients at first relapse vs second relapse are presented in Table 2.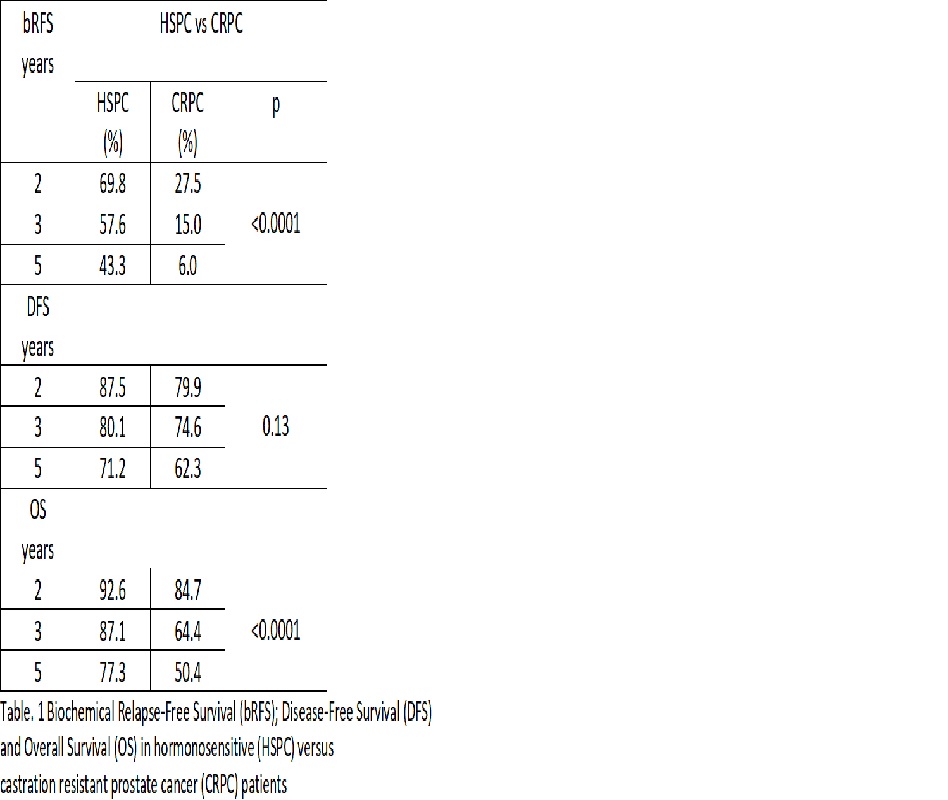
Conclusion
In our large cohort of patients treated with ENRT and PET-guided SIB for LNM, with a long follow-up, CRPC patients and patients with second relapse after surgery already treated with ART/SRT have a significantly worse evolution than patients still HSPC, or at the first relapse after surgery.