Total neoadjuvant therapy for rectal cancer – Experience of the Carlos Van Buren Hospital
Jose Antonio Solis Campos,
Chile
PO-1405
Abstract
Total neoadjuvant therapy for rectal cancer – Experience of the Carlos Van Buren Hospital
Authors: Gabriel Lazcano Álvarez1, Ilan Perrot Rosenberg2, Jose Solis Campos1, Benjamin Tudela1, Gabriel Veillon Contreras1, Lisset Gonzalez Abascal1
1Universidad de Valparaiso, Radiation Oncology, Valparaiso, Chile; 2Hospital Carlos Van Buren, Radiation Oncology, Valparaiso, Chile
Show Affiliations
Hide Affiliations
Purpose or Objective
Total neoadjuvant therapy (TNT) is an approach consisting in the delivery of radiotherapy and systemic chemotherapy in their entirety before surgery. It’s one of the current standards for the treatment of locally advanced rectal cancer (LARC). The purpose of this study is to describe the result of TNT at the Carlos Van Buren Hospital (Valparaíso, Chile).
Material and Methods
This retrospective cohort includes patients treated with curative intent for LARC between 2017 and 2021. TNT was administered as short course radiotherapy with a prescription of 25 Gy in 5 daily fractions, followed by medical oncologist’s choice of FOLFOX or XELOX, then surgery.
Overall survival is measured from start of radiotherapy. As follow-up of previous work (PO-1322 at ESTRO 2022), neoadjuvant rectal (NAR) score, initially proposed by George et al. (2015), was calculated for patients with available clinical and surgical staging and modelled against death events up to 36 months using logistic regression and ROC curve analysis. Statistical analysis was made in Stata v17 (Statacorp, 2022).
Results
The current cohort includes 107 patients. Initial local staging was reported as cT2 in 6.6% of patients; cT3 in 69.8% and cT4 in 23.6%, with an 84% of nodal involvement (cN1-2). All patients were staged with a CT scan, and 85% had a pelvic MRI.
Median duration of radiotherapy was 5 days (IQR 5-7), with a median interval between end of radiotherapy and surgery of 112 days (IQR 94-150). In between, a median of 3 cycles of chemotherapy were administered (IQR 2-3).
Surgical staging was retrieved for 81 patients, reporting 24.7% ypT0 patients; 4.9% ypT1; 17.3% ypT2; 43.2% ypT3 and 9.9% ypT4. Nodal staging was ypN0 in 76,5%. Overall, 21% were staged as ypT0N0, also denominated complete pathological response (pCR).
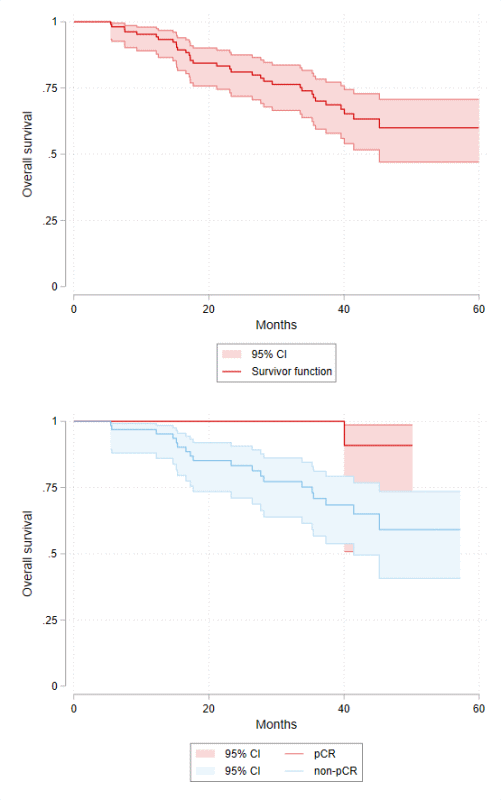
Median follow-up was 36.7 months (IQR 21.1-42.5), with a 3-year overall survival of 69.9% (CI 95% 59.3-78.3). Patients with available surgical biopsy had a 3y-OS of 76.9% (CI 95% 64.9-85.3); those achieving a pCR had a 3y-OS of 100%, registering a single event at 40-months. By comparison, patients without a pCR had a 3y-OS of 70.7% (CI 95% 56.4-81) (p-logrank = 0.0405). (Figure 1)
Figure 1.- OS for the whole cohort and by pCR
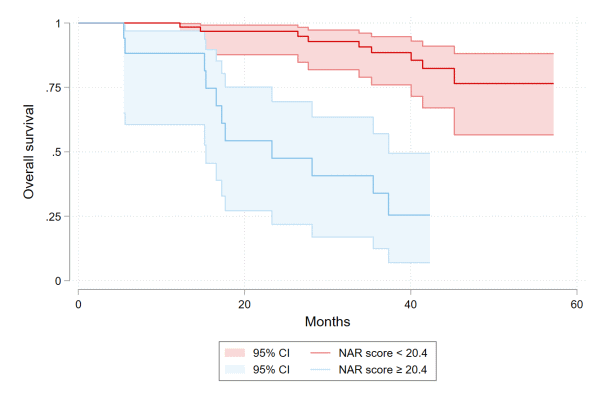
NAR score was calculated for 81 patients. A first model including only NAR score had an area under curve (AUC) of 0.81; NAR score had a coefficient of 0.076 (CI 95% 0.028-0.125, p = 0.002). Owing to the intrinsic relation between low NAR score and pCR, a second model omitting the later patients was created. AUC of the second model was 0.74 with a coefficient of 0.062 (CI 95% 0.014-0.110, p = 0.002). The optimal cutoff point was estimated to be 20.4, with a Youden index of 0.52. Patients with NAR score < 20.4 had a 3y-OS of 88.5% (CI 95% 76-94.7) vs 33.9% (CI 95% 12.5-57.1) for NAR score ≥ 20.4 (p-logrank < 0.0001) (Figure 2).
Figure 2.- OS by NAR score
Conclusion
TNT is an effective treatment, exhibiting excellent results in the patients achieving pCR. NAR score offers good discrimination for 3y-OS.