Initial experience of rectum SIB radiotherapy on the Unity MR-Linac
Hubert Stankiewicz,
United Kingdom
PO-1400
Abstract
Initial experience of rectum SIB radiotherapy on the Unity MR-Linac
Authors: Hubert Stankiewicz1, Joan Chick1, Manasi Ingle2, Adam Mitchell1, Helen Barnes3, Trina Herbert3, Simeon Nill1, Uwe Oelfke1, Brian Ng-Cheng-Hin2, Shreerang Bhide2, Alex Dunlop1
1The Royal Marsden NHS Foundation Trust and The Institute of Cancer Research, The Joint Department of Physics, London, United Kingdom; 2The Royal Marsden NHS Foundation Trust and The Institute of Cancer Research, Radiotherapy, London, United Kingdom; 3The Royal Marsden NHS Foundation Trust, Radiotherapy, London, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
A 2-phase rectum simultaneous integrated boost (SIB) treating 52.5/45Gy to the primary and elective targets in 25 fractions (#) was implemented. This enables initial boosting of the primary target using MRgART on the Unity MR-linac (MRL, Elekta AB, Stockholm) with 16.5/9Gy/5# to the primary and elective targets and subsequent elective non-adaptive treatment on C-arm linac (36Gy/20#). This approach utilises the superior MR visualisation to ensure accurate daily adaptation to the primary target by accounting for large interfraction motion. The aim of this work is to present the initial experience for the MRL-delivered fractions for the first 5 patients.
Material and Methods
5 patients treated for rectal cancer under an institutional study (PERMIT trial; NCT03727698) were selected for analysis. Targets volumes were defined as per RCR guidelines [1]. MRL reference plans using an 11-field step and shoot IMRT delivery were created on pre-treatment reference images to meet OAR dose constraints. RCR OAR dose constraints were split between the MRL and C-arm phases in the ratio of 16.5:36 (Monaco 5.40.01). Online adaptation of the reference plan followed an Adapt to Shape (ATS) workflow, with the option of subsequent Adapt to Position (ATP of ATS) if the primary target had moved more than 5mm. We determined the overall treatment session times and the % of dose constraints that were achieved for all online adaptive SIB plans.
Results
All MRL adaptive ATS SIB plans were successfully optimised and approved by a clinician for treatment. 24/25 plans met all mandatory dose constraints for PTV coverage. The high-dose PTV (PTV1650) V95%>95% dose constraint was not met in one ATS plan (94.8%) due to preferentially sparing adjacent small bowel. The mean PTV1650 V95% across all online ATS plans was 98.4%, with no individual patient mean V95% less than 96.4%. The mean low-dose PTV V95% across all online plans was 99.2%, with all individual patient mean V95% above 98.8%. 99.5% of all online OAR mandatory constraints were met for ATS plans.
Two ATP of ATS plans were required. All mandatory dose constraints were met in both ATP of ATS plans.
The median time on couch was 41.3min with a range of individual patient mean time: 35.4–54.4min, reflecting variability in plan complexity in terms of volume delineation and optimisation. The median (range) time between online contouring and treatment delivery was 23.5min (20.6–38.3min). The median (range) treatment delivery time for all online plans was 8min (7–8.6min).
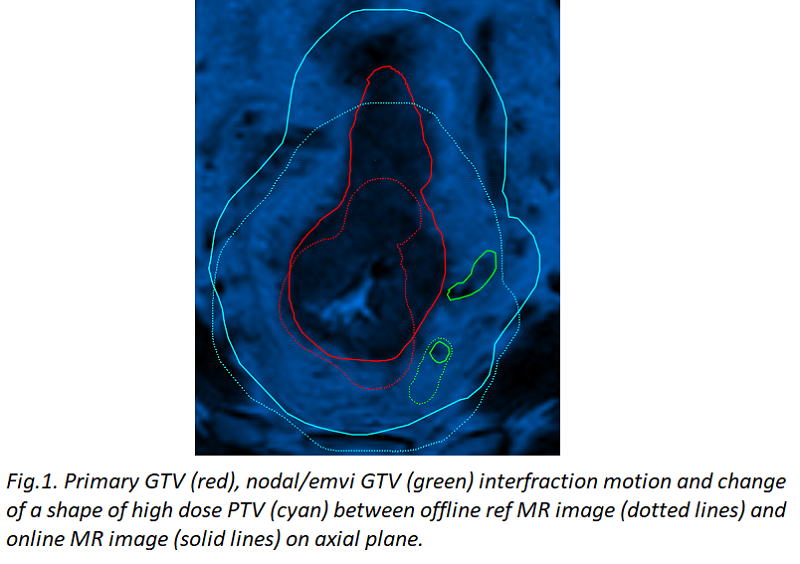
Figure 1 illustrates an example of the interfraction motion observed for these patients and shows potential undercoverage of the primary GTV for non-adaptive treatment.
Conclusion
MRgART for Rectum Cancer on the MRL is feasible and can account for large interfraction changes observed for this indication. Toxicity and pathological outcomes will be presented later. To leverage the full potential of MRgART for rectal cancer, dose escalation strategies or PTV margin reduction could be considered for ATS workflows.