Bowel delineation methods and prediction of acute and late diarrhea in radiotherapy of anal cancer
Katrine Smedegaard Storm,
Denmark
PO-1399
Abstract
Bowel delineation methods and prediction of acute and late diarrhea in radiotherapy of anal cancer
Authors: Katrine Smedegaard Storm1, Sif Homburg1, Gitte F Persson1,2, Claus P Behrens1,3, Patrik Sibolt1, Karen-Lise Garm Spindler4,5, Camilla Kronborg6,7, Eva Serup-Hansen1
1Copenhagen University Hospital - Herlev and Gentofte, Department of Oncology, Copenhagen, Denmark; 2University of Copenhagen - Faculty of Health Sciences , Department of Clinical Medicine, Copenhagen, Denmark; 3Technical University of Denmark, Department of Health Technology, Roskilde, Denmark; 4Aarhus University Hospital, Department of Experimental Clinical Oncology, Aarhus, Denmark; 5Aarhus University Hospital, Department of Oncology, Aarhus, Denmark; 6Danish Centre for Particle Therapy, ., Aarhus, Denmark; 7Aarhus university, Department of Clinical Medicine, Aarhus, Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
Concomitant chemo-radiotherapy is the standard of care for anal cancer. The treatment is associated with significant acute- and late gastro-intestinal (GI) toxicity.
Several studies have shown a correlation between GI toxicity and the volume of irradiated bowel. However, bowel delineation is not consistent in different clinical trials and this affects the recommended dose constraints and makes comparison difficult. Constraints are mainly applied for acute toxicity, but patients also experience late GI toxicity impacting their quality of life.
Plan-A is a prospective, national Danish trial evaluating toxicity, that included patients with anal cancer treated with VMAT/IMRT-planned chemo-radiotherapy from 2015-2021.
The purpose of this study is to evaluate which bowel delineation approach leads to the optimal prediction of acute and late diarrhea in patients with anal cancer receiving concomitant chemo-radiotherapy
Material and Methods
69 patients were included for analysis. Acute toxicity was registered at baseline, mid- and end of treatment (EOT), and 2-weeks after EOT. Late toxicity was registered at one year after EOT, both using CTCAE v. 4.
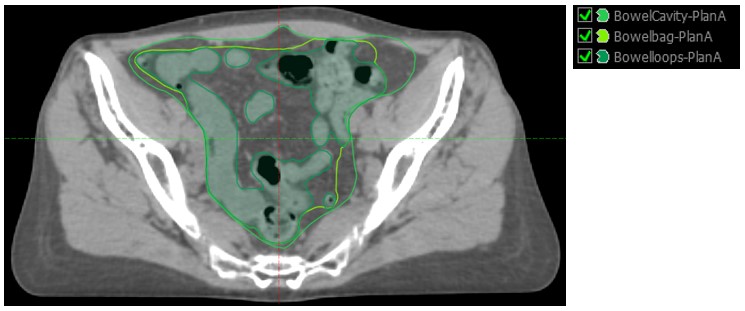
Bowels were retrospectively delineated on the planning CT as 1) Bowel cavity; including the entire peritoneal cavity from lower limit of L4 to last visible bowel loop as per RTOG, 2) bowel bag; part of the peritoneal cavity including bowel loops and 3) individual bowel loops (Figure 1). V15Gy, V30Gy and V45Gy were determined for the different bowel delineations and compared to toxicity scores. Difference between toxicity and dosimetric values was evaluated using Mann-Whitney test.
Results
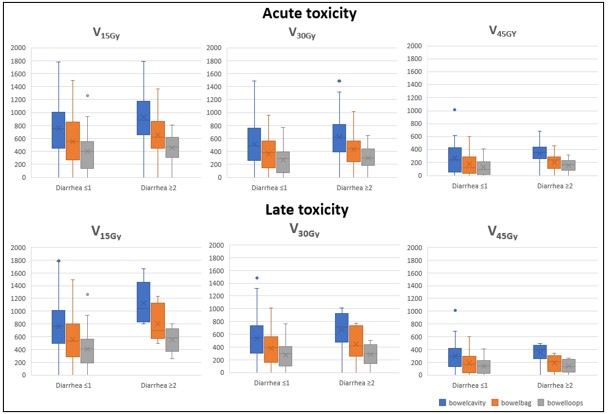
Peak acute grade ≥2 diarrhea was seen in 28 (40.6%) of 69 patients and late toxicity was seen in 6 (9.4%). One-year CTCAE was available for 93%. Median [IQR] volume was 1517.3 cm3 [1169.7;2025.6] for bowel cavity, 1125.1 cm3 [864.8;1431.3] for bowel bag and 813.6 cm3 [634.9;1008.0] for bowel loops. Figure 2 shows boxplots of V15Gy, V30Gy and V45Gy for bowel cavity, bowel bag and bowel loops, for patients with grade 0-1 and ≥2 acute and late diarrhea.
For all evaluated parameters vi found larger bowel volumes with higher toxicity grade, however none reached significance. The most pronounced difference was seen for bowel cavity V15 for both acute and late toxicity. Median [IQR] V15Gy for patients with no acute diarrhea was 747.4 cm3 [480.3;1006.3]and 883.9 [673.6;1118.2] for patients with grade ≥2 (p=0.095). Median [IQR] V15Gy for patients with no late diarrhea was 802.4 cm3 [504.6;1015.9] and 834.1 cm3 [662.5;1457.3] for patients with grade ≥2 (p=0.053).
Conclusion
Acute and late diarrhea is still significant with modern radiotherapy for anal cancer. There was a trend for higher toxicity with higher irradiated volumes, but insignificant for all delineation methods, however V15Gy showed most promise for both acute and late diarrhea.