Neoadjuvant short-course RT or chemoradiation plus consolidation chemotherapy for rectal cancer
Shing Fung Lee,
Singapore
PO-1392
Abstract
Neoadjuvant short-course RT or chemoradiation plus consolidation chemotherapy for rectal cancer
Authors: Shing Fung Lee1,2, Pui Lam Yip2, Balamurugan A Vellayappan1, Harvey J Mamon3, Francis Ann-Shing Lee2
1National University Cancer Institute, Radiation Oncology, Singapore, Singapore; 2Tuen Mun Hospital, Clinical Oncology, Hong Kong, Hong Kong (SAR) China; 3Brigham and Women’s Hospital / Dana Farber Cancer Institute, Radiation Oncology, Boston, USA
Show Affiliations
Hide Affiliations
Purpose or Objective
Evidence comparing pre-operative short-course radiotherapy (SCRT) versus neoadjuvant chemoradiation (NCRT), both followed by consolidation chemotherapy before radical rectal surgery is limited. We performed a retrospective cohort study to compare the two treatment strategies in terms of treatment response, survival outcomes, and toxicity.
Material and Methods
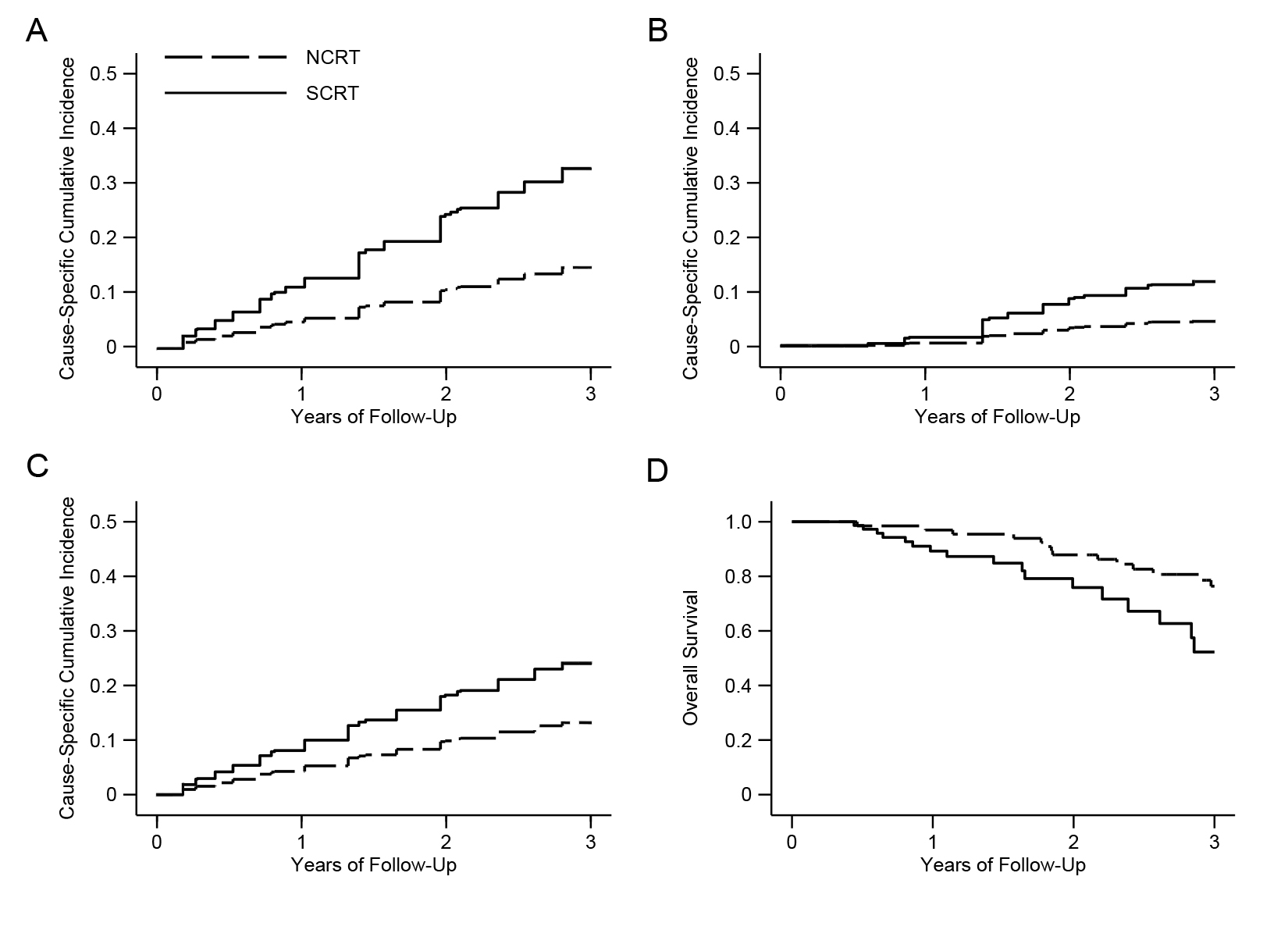
We identified locally advanced rectal cancer (cT3–4 and/or N+) who received SCRT or NCRT with consolidation chemotherapy followed by total mesorectal excision between 2013 and 2021. We evaluated the cause-specific cumulative incidence of disease-related treatment failure , locoregional recurrence, distant metastases, and overall survival by using flexible parametric competing risk analysis and Kaplan-Meier methods as appropriate and adjusting for treatment regimens, and clinicopathological factors. Treatment response including pathological complete response (pCR), and tumor downstaging, and toxicity were reported.
Results
We analyzed 144 patients in which 115 (80%) underwent curative rectal surgery. 42 (76%) patients in the NCRT and 45 (75%) in the SCRT group had sphincter preserving surgery . pCR was achieved in 10 (18%) and 7 (12%) patients in NCRT and SCRT groups respectively (odds ratio, 1.68; 95% confidence interval [CI], 0.59–4.78; P = 0.329). The adjusted cause-specific hazard ratio (HR) for disease-related treatment failure in patients treated with NCRT compared with SCRT was 0.31 (95% CI, 0.11–0.85; P = 0.024). The 3-year cumulative probability of disease-related treatment failure was 14.7% in the NCRT group vs 32.9% in the SCRT group. 3-year overall survival (87.9% vs 52.3%) was significantly better in the NCRT group (HR, 0.32; 95% CI, 0.10–0.99; P = 0.048). No significance difference in T-downstaging, N-downstaging, significant pathologic downstaging (ypT0-2N0), locoregional control and distant metastasis was detected. Thrombocytopenia and gastrointestinal toxicity were the most common preoperative grade ≥3 hematologic and non-hematologic toxicity, respectively. Grade ≥3 late rectal toxicity occurred in 10 (15%) patients in the NCRT group versus 2 (3%) in the SCRT group.
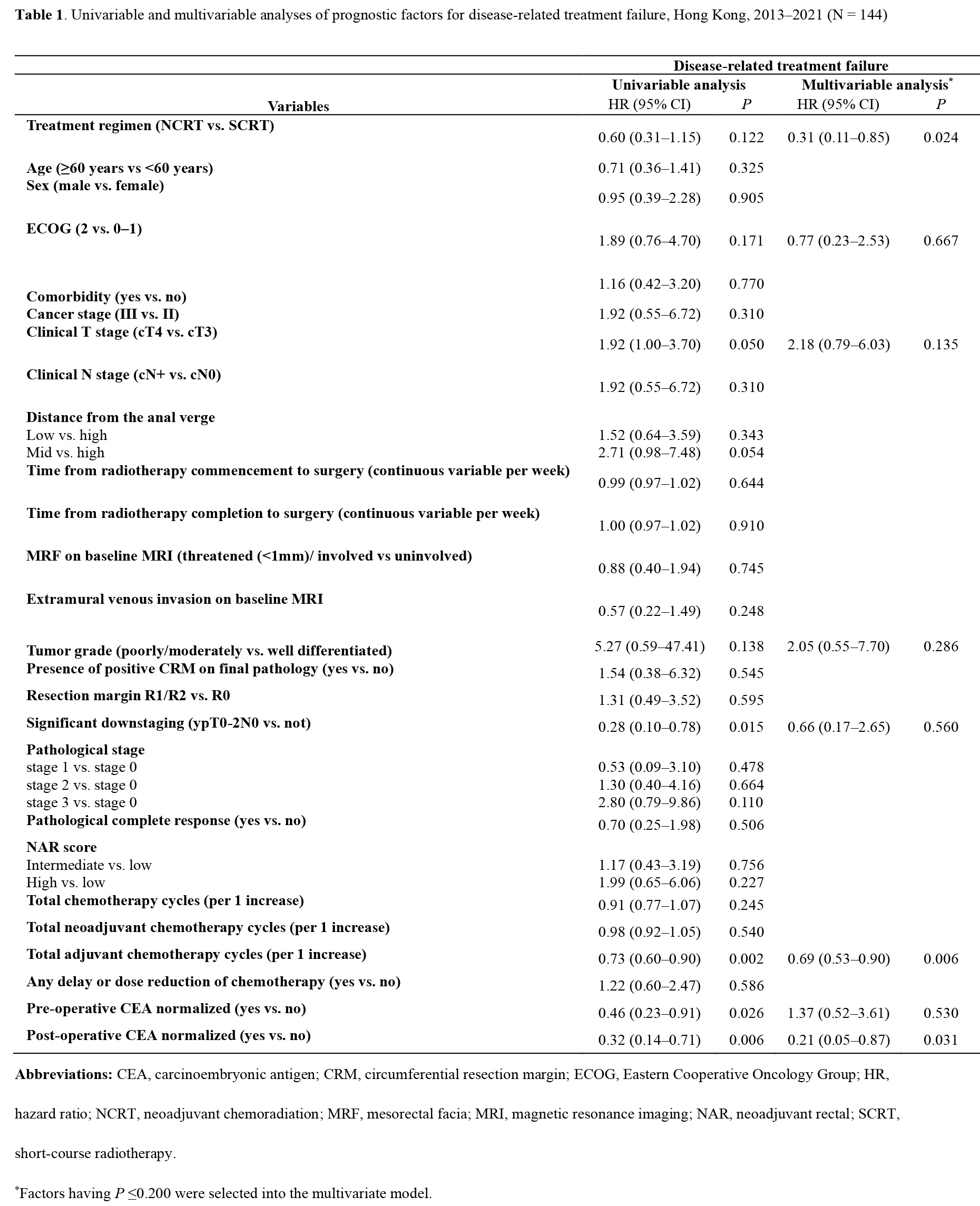
Figure 1. Cause-specific cumulative incidence of disease-related treatment failure (A), locoregional failure (B), and distant metastases (C), and overall survival curve (D).
Conclusion
Based on our cohort, patients treated with NCRT and consolidation chemotherapy had a improved disease-related treatment failure and overall survival, despite a higher late rectal toxicity. Further studies to evaluate the long-term survival outcomes and toxicity are needed.