The efficacy of Stereotactic Body Radiotherapy (SBRT) in liver metastases, single-center experience
Ahmed Allam Mohamed,
Germany
PO-1377
Abstract
The efficacy of Stereotactic Body Radiotherapy (SBRT) in liver metastases, single-center experience
Authors: Ahmed Allam Mohamed1, Marie Berres2, Christian Trautwein2, Martin Kirschner3, Sven Lang4, Ulf Neumann4, Philipp Bruners5, Michael Eble1
1University Hospital RWTH Aachen, Department of Radiation Oncology, Aachen, Germany; 2University Hospital RWTH Aachen, Department of Gastroenterology, Hepatology and infectious Diseases, Aachen, Germany; 3University Hospital RWTH Aachen, Department Hematology, Oncology, Hemastology and Stem Cell Transplantation, Aachen, Germany; 4University Hospital RWTH Aachen, Aachen, Department Visceral and Transplantation Surgery, Aachen, Germany; 5University Hospital RWTH Aachen, Department Diagnostic and interventional Radiology, Aachen, Germany
Show Affiliations
Hide Affiliations
Purpose or Objective
Liver metastases are the most common liver tumors. In the oligometastatic stage, surgical resection is the standard approach. Alternatives are local ablation (Radiofrequency and microwave ablation) or radio-ablation using the SBRT. We planned this single-center analysis to report the outcomes and toxicity of SBRT for liver metastases.
Material and Methods
Patients with oligometastatic cancer, who received SBRT as an ablative tool for their liver metastasis and received at least one follow-up were included in the analysis. Excluded from the analysis are patients who received radiation in palliative settings to control symptoms (pain and biliary obstruction).
Results
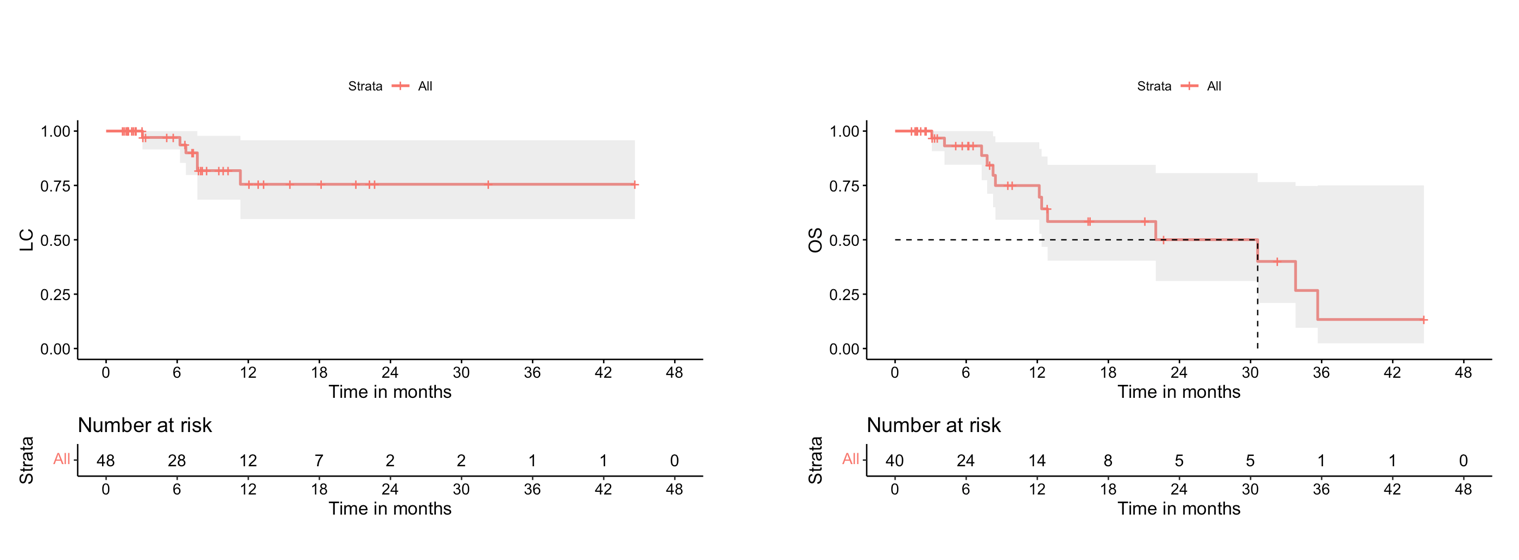
We identified 56 patients, who received SBRT for liver metastases between 2013-2022 in our local registry. Sixteen patients were excluded (10 patients received a palliative dose for symptom control in the polymetastatic stage and 6 patients did not receive follow-up in our center until the analysis). Forty Patients with 48 lesions were included in the analysis (23 patients with colorectal cancer, 5 with pancreatic cancer, 4 with Lung cancer, and 8 other malignancies). The median prescribed dose to PTV as EQD2/10 was 70.3 Gy (49.6-93.8) in median 5 fractions (3-12). SBRT was applied as image-guided radiation in all patients and fiducial markers were used in a subset of patients starting from the year 2018. The median follow-up and median overall survival were 7.5 and 30.6 months, respectively, and the local control (LC) at 6, 12, and 24 months were 97.1%, 75.5% & 75.5%. respectively.
None of the patients experienced radiation-induced disease “RILD”. No grade 4 or 5 toxicity was observed after SBRT. Grade 3 toxicity was diagnosed in 2 patients (5%), one with isolated elevation gamma-Glutamyl transferase without symptoms of biliary obstruction, and the other patient required a biliary stent for biliary stenosis.
Conclusion
Our single-center experience confirms SBRT as a reliable ablative tool in liver metastases with an acceptable low rate of grade ≥ 3 toxicity.