stereotactic radiotherapy for oligometastatic esophagogastric carcinoma outcome, prognostic factors
Luciana Di Cristina,
Italy
PO-1364
Abstract
stereotactic radiotherapy for oligometastatic esophagogastric carcinoma outcome, prognostic factors
Authors: Luciana Di Cristina1,2, Davide Franceschini1, Maria Ausilia Teriaca1, Veronica Vernier1,2, Lorenzo Lo Faro1,2, Ciro Franzese1,2, Tiziana Comito1, Elena Clerici1, Luisa Bellu1, Luca Dominici1, Ruggero Spoto1, Maria Massaro1, Pierina Navarria1, Marta Scorsetti1,2
1IRCCS Humanitas Research Hospital, Radiotherapy and Radiosurgery, Rozzano – Milan, Italy; 2Humanitas University, Biomedical Sciences, Pieve Emanuele – Milan, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
The aim of this study was to evaluate clinical results and prognostic factors in a cohort of patient with oligometastatic esophagogastric adenocarcinoma treated with SRT.
Material and Methods
The study included patients affected by 1 to 3 metastases treated with SRT from 2013 to 2021. Local control (LC), overall survival (OS) and progression free survival (PFS) were evaluated. We also estimated time to polymetastatic dissemination (TTPD) in patients experiencing a further disease progression and time to systemic therapy change/initiation (TTS).
Results
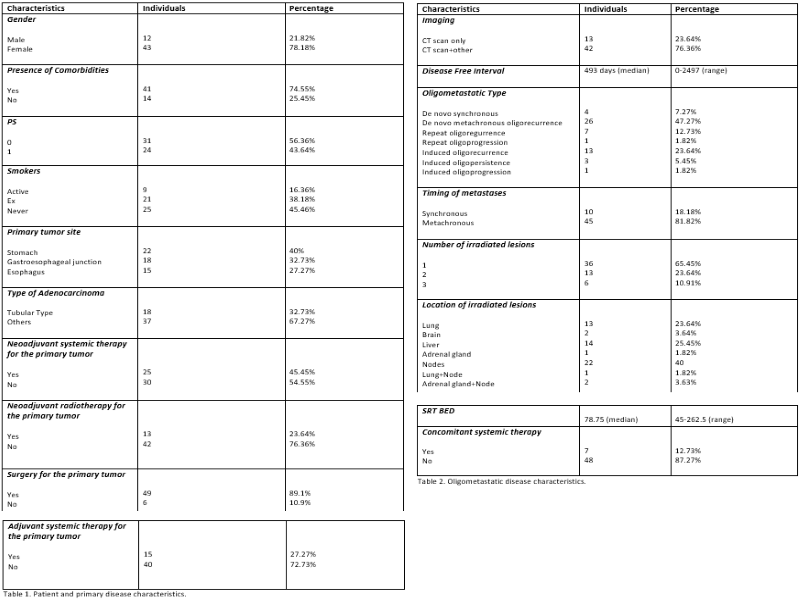
Between 2013 and 2021, 55 patients were treated with SRT on oligometastatic sites. Median age was 69 years. Primary tumor, patients and oligometastatic disease characteristics are shown in table 1 and 2. We observed 21 complete response (CR); 24 partial response (PR); 8 stable disease (SD) and 2 progressive disease (PD).
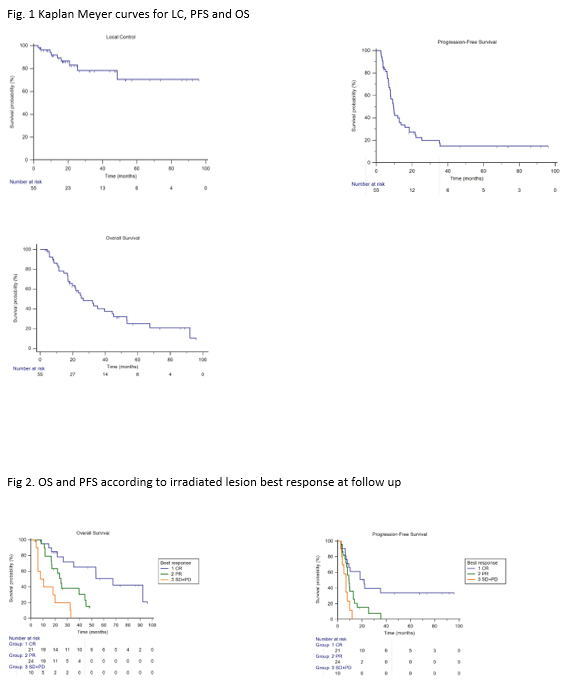
Median follow-up was 20 months. Nine patients had local progression, median LC was not reached. 1 and 3 years LC was respectively 92% and 78%. Forty-one patients experienced further distant disease progression, median PFS was 9.7 months, 1 and 3 years PFS was respectively 40% and 15%. Thirty-four patients died, median OS was 26.6 months, 1 and 3 years OS was respectively 78% and 40% (fig.1).
During follow up, 24 patients changed or initiated a new systemic therapy, median TTS time was 9 months. Twenty-seven patients experienced poliprogression, 44% after 1 year and 52% after 3 years. Median TTPD was 8 months.
At univariate analysis disease free interval, timing of metastases, performance status (PS) and local response (LR) influenced PFS. The best LR was related with prolonged PFS on multivariate analysis: CR vs PR+SD+PD (HR 0.36 95%CI 0.17-0.76 p=0.008) and SD+PD vs CR+PR (HR 2.36, 95%CI 1.02-5.59; p=0.04). Also timing of metastases (synchronous vs metachronous: HR 3.07, 95%CI 1.50-6.26; p=0.002) and PS (ECOG 1 vs 0: HR 2.10, 95% CI 1.10-3.97; p=0.02) were confirmed in multivariate analysis. LR and BED >75 Gy correlated with OS at univariate analysis; only LR maintained significance at multivariate analysis (p<0.0001) (fig 2).
Conclusion
SRT represents a valid treatment for oligometastatic esophagogastric adenocarcinoma, with promising LC and OS at 3 years. CR correlated with PFS and OS, while metachronous metastasis and a good PS correlated with a better PFS. Future studies are needed to study the integration between SRT and systemic therapies.