Pattern of failure after stereotactic body radiotherapy to liver metastases: impact of local control
PO-1354
Abstract
Pattern of failure after stereotactic body radiotherapy to liver metastases: impact of local control
Authors: Andrea Gaetano Allegra1, Mauro Loi1, Lucia Angelini1, Ilaria Bonaparte1, Niccolò Bertini1, Giulio Frosini1, Carolina Orsatti1, Marianna Valzano1, Pierluigi Bonomo1, Gabriele Simontacchi1, Giulio Francolini1, Beatrice Detti1, Vanessa Di Cataldo1, Luca Visani2, Viola Salvestrini2, Livia Marrazzo3, Margherita Zani3, Laura Masi4, Raffaella Doro4, Lorenzo Livi1
1Azienda Ospedaliero Universitaria Careggi, Università di Firenze, Radiation Oncology, Florence, Italy; 2Istituto Fiorentino di Cura e Assistenza (IFCA), CyberKnife Center, Florence, Italy; 3Azienda Ospedaliero Universitaria Careggi, Università di Firenze, Medical Physics Unit, Florence, Italy; 4Istituto Fiorentino di Cura e Assistenza (IFCA), Department of Medical Physics, Florence, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Surgical resection of liver metastases (LM) may be feasible for only 30% of patients due to unfavourable location, disease burden or comorbidities. There’s evidence of excellent local control (LC) and low toxicity in patients treated with stereotactic body radiotherapy (SBRT) but data on global disease control are scarce. The objective of this preliminary analysis was to assess patterns of failure in a cohort of patients treated with SBRT to LM.
Material and Methods
Data from patients treated between 2018 and 2020 at a single Institution with SBRT to LM were collected. Patients received an EQD2 of at least 50 Gy (α/β=10) as per ESTRO consensus. Failure patterns after SBRT defined as local relapse (LR), intrahepatic relapse (out of field, IHR) and extrahepatic relapse (EHR), as well as Local Control (LC) and Overall Survival (OS) rates, were evaluated.
Results
Forty-three patients with liver-only metastatic disease received SBRT. Most common primary tumors were breast cancer (n=18.42%) and colon cancer (n=10.23%). SBRT was performed using Cyberknife real-time tumor tracking (n=30,70%) or abdominal compression-assisted VMAT (n=13.30%) delivering 35-60 Gy in 3-5 fractions, corresponding to median EQD2 of 94 (50-150) Gy. Twelve (28%) patients were chemotherapy-naïve, while the remaining patients received 1 (20,46%), 2 (5,12%) or ≥3 (6,14%) chemotherapy lines. Median follow-up was 12 months. Patterns of failure are reported in Table 1.
| +LR | +IHR | +EHR | +IHR+EHR |
| LR | 0 | 12 | 0 | 9 |
| IHR | 12 | 2 | 11 | / |
| EHR | 0 | 11 | 5 | / |
| IHR+EHR | 9 | / | / | / |
Table 1.
One-year OS was 87%. At multivariate analysis LC was significantly correlated with EQD2≥94Gy (p=0.009) and ≥3 chemotherapy lines (p=0.04). IHR and EHR were significantly associated with local failure (p=0.0013) and intrahepatic progression (p=0.03), respectively. A significant correlation between OS and local relapse was shown (p=0.026). Kaplan-Meier curves for these analyses are shown in Figure 1.
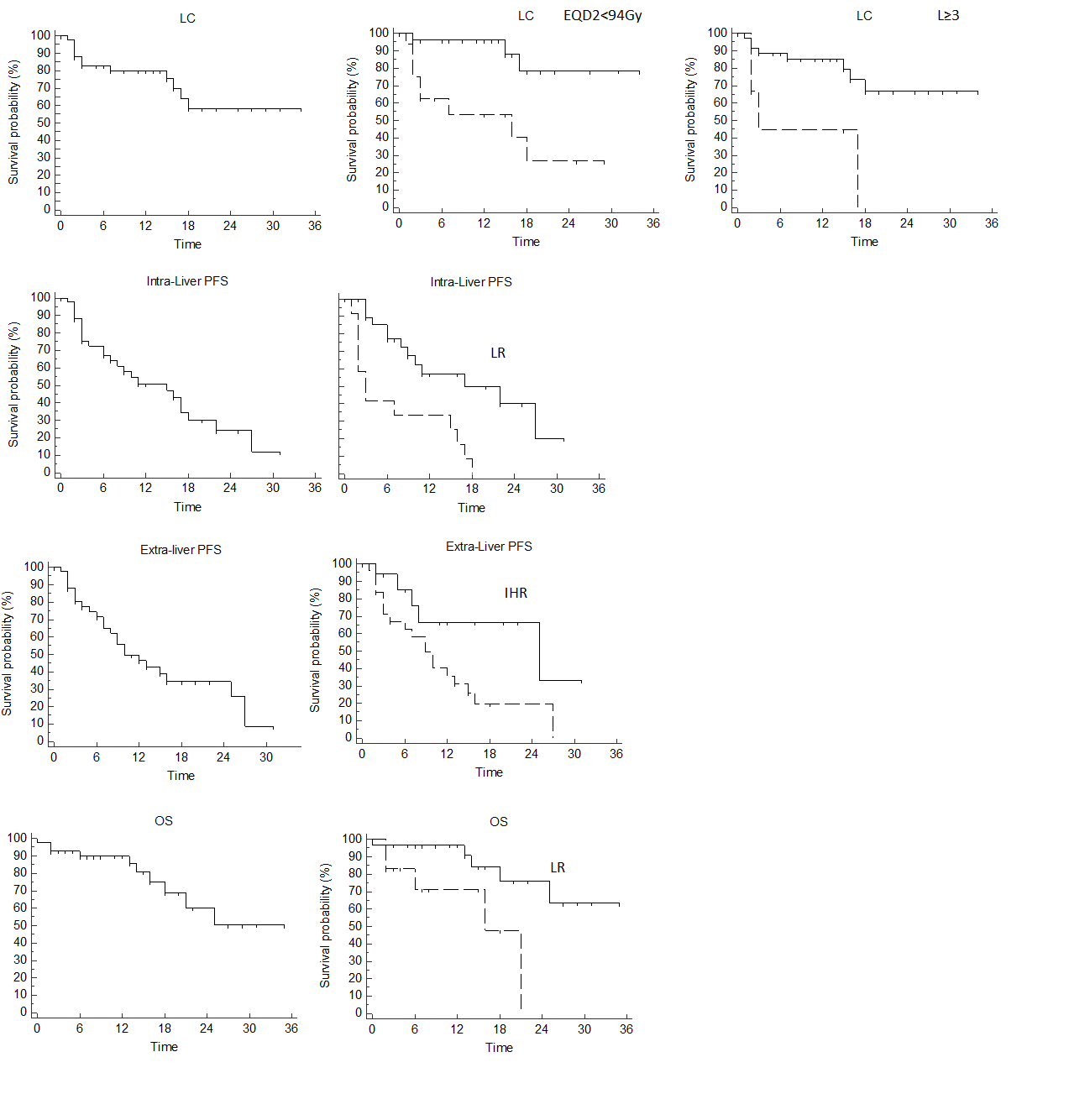
Figure 1.
Conclusion
In our experience, improved LC using high BED in non-heavily pretreated patients was correlated to reduced risk of IHR and to improved OS. IHR was the most common mode of failure in patients treated with SBRT for LM and was correlated with further extrahepatic progression. Our findings suggest that IHR may result from uncontrolled macroscopic LM rather than ubiquitous micrometastatic dissemination, and preceed further systemic spread at distant sites. Our findings support the use of SBRT as an efficient tool to block stepwise metastatic spread from uncontrolled isolated LM to liver, and from liver to distant site, thus extending global disease control.