Is EDIC a metric to predict lymphopenia in oesophageal cancer patients?
PO-1352
Abstract
Is EDIC a metric to predict lymphopenia in oesophageal cancer patients?
Authors: Filippos Apostolopoulos1, Owen Nicholas2, Rebecca Slinger1
1South West Wales Cancer Centre, Swansea Bay University Health Board, Department of Medical Physics and Clinical Engineering, Swansea, United Kingdom; 2South West Wales Cancer Centre, Swansea Bay University Health Board, Department of Oncology, Swansea, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
The spleen has not traditionally been considered an organ at risk (OAR) when treating oesophageal cancer (OEC) with radiotherapy. However, studies have shown that mean spleen dose (MSD) higher than 10 Gy is associated with increased rates of infection and infection-related mortality and patients that receive doses higher than 40 Gy are at a substantially higher risk [1]. Radiation-related lymphopenia is one of the risks associated with spleen irradiation during radiotherapy and is related to poorer overall survival [2]. The purpose of this study is to evaluate a metric which could predict the grade of lymphopenia and the overall survival rate of oesophageal cancer patients based on this data.
Material and Methods
Patients at our centre from August 2018 to December 2019 (n = 41) who were treated with VMAT for OEC > 45 Gy and 25 fractions were audited and analysed.
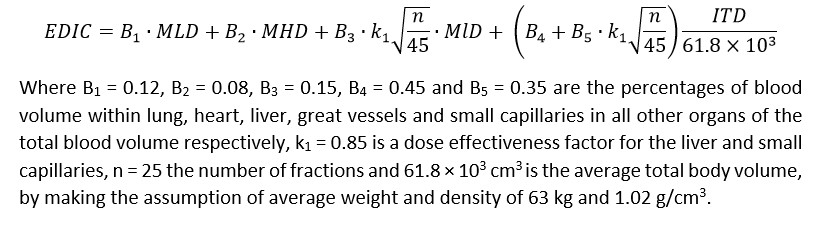
Effective Dose to Immune Cells (EDIC) [3] and MSD were collected to observe any correlation between lymphopenia grade, lymph blood values pre and post treated (PRTL and POTL respectively) or PTV volume. EDIC is calculated based on the major blood containing organs in the human body (lungs, heart, liver) and the integral dose which in our study was calculated by truncating the external contour 3 slices above the lungs and 3 slices below the kidneys to maintain consistency in the calculations.
For our statistical analysis we used two methods: the Spearman Correlation and Linear Regression.
Results
Total of 41 patients. 78% of them (32/41) had a mean splenic dose > 10 Gy with no patient receiving more than 40 Gy. MSD (median = 1527.5 cGy) and PTV volume (median = 468.9 cm3) were collected for all patients, the EDIC was calculated (median = 630.2 cGy) and the data is represented in the table below.
| Variable | Spearman Correlation POTL (p-value) | Linear Regression POTL (p-value) |
| MSD | 0.442 | 0.747 |
| EDIC | 0.935 | 0.924 |
| PTV | 0.248 | 0.607 |
Conclusion
No significant associations were found no matter the statistical method used. In both approaches the p-value is significantly large which indicates no correlation between the analysed variables. The main limitation is the small sample, and there is no clear indication that higher spleen dose nor EDIC is associated with higher grade of lymphopenia. Previous work has shown EDIC > 4 Gy results in G4 lymphopenia but this is not replicated in this study. No indication that there is value in reducing splenic dose to improve lymphopenia rates.
References