Chest Wall toxicity after lung SBRT treatments and influential parameters.
Sandra Fernandez Alonso,
Spain
PO-1320
Abstract
Chest Wall toxicity after lung SBRT treatments and influential parameters.
Authors: GUSTAVO POZO RODRIGUEZ1, ANA MILANES GAILLET1, SANDRA GUARDADO GONZALEZ2, SANDRA FERNÁNDEZ ALONSO2, IVAN ALONSO DELGADO3, DANIEL MARTIN GARCIA3, PEDRO ADAIMI HERNANDEZ3, RAUL DIAZ FUENTES3, PALOMA BOTELLA FAUS1, ANGEL GAITAN SIMON3, MARTA MANZANO RODRIGUEZ3, SARA PEDRAZA FERNANDEZ4, NIEVES GASCON COSTOSO4, EDUARDO CABELLO MURILLO3
1H.U. 12 DE OCTUBRE, MEDICAL PHYSICS, MADRID, Spain; 2H.U. 12 DE OCTUBRE, RADIATION ONCOLOGY, MADRID, Spain; 3H.U.12 DE OCTUBRE, MEDICAL PHYSICS, MADRID, Spain; 4H.U.12 DE OCTUBRE, RADIATION ONCOLOGY, MADRID, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
To quantify the fraction of patients that underwent SBRT of lung and have exhibited chest wall toxicity after treatment, and its association with influential parameters.
Material and Methods
Cohort of 50 SBRT lung patients treated in our institution were selected filtering by target location and only considering those abutting or invading chest wall (CW).
SBRT treatments were performed on a Varian Clinac 2300 iX linear accelerator. It includes an On Board Imager unit to perform KVCBCT and a Millenium 120 MLC (5mm thickness at isocenter) for treatments performance (Varian Medical Systems, Palo Alto CA).
Treatment Planning System used for clinical dosimetry was Eclipse 15.6, and two algorithms available: Acuros 15.6 and AAA 15.6 (Analytical Anisotropic Algorithm) configured with a 2.5 mm calculation grid . PO 15.6 optimizer was used for VMAT treatments.
4DCT was acquired with Philips Brilliance CT, using a nominal slice thickness of 2mm. Respiratory cycle was binned into 10 phases and ITV was generated by means of merging 10 segmented GTV.
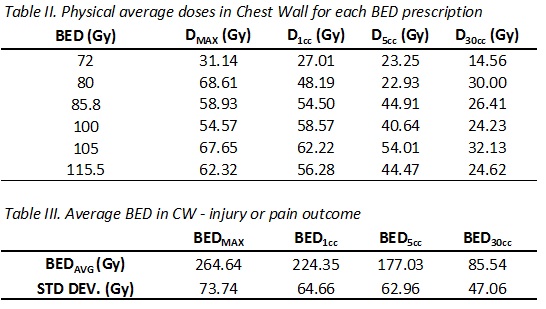
Prescription BED to PTV ranged from 72 to 115.5Gy, and dosimetric chest wall parameters were extracted from DVH curves.
In our institution, patient medical history is stored in natural language format. To identify those patient who suffer any kind of toxicity after SBRT, the search included these keywords: ‘rib cage pain’ OR ‘fracture’ OR ‘cleft bone’ OR ‘callus’.
Results
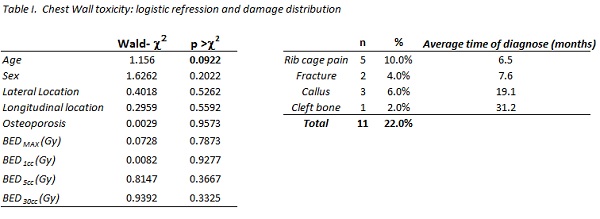
A logistic regression has been performed with Stata v.16 (StataCorp.) to evaluate the influence of age, sex, location, bone density (osteoporosis) and BED metrics in CW toxicity (table I), finding no significant association. In agreement with UK Consortium and AAPM TG101, BED calculation has considered dose to volume constrains as shown in table II and III.
Up to 22% of cases presented any kind of chest wall toxicity: 12% concerning CW injury and at least 10% developed rib cage pain.
Only 8% of patients (2 female and 2 male) registered osteoporosis in their reports, coherent with Spanish prevalence for female and male > 50 years old.
Time of diagnose ranged from 6.4 to 31.2 months (fracture, callus or cleft bone) and from 1.7 to 19.5 months (emerging pain).
Conclusion
22% of patients that have undergone lung SBRT treatments in our institution developed pain or CW injury.
Although high doses, aged patients and presence of osteoporosis seem to work in favour of CW toxicity, no apparent correlation has been found in our study.
Structured information might be the standard way of reporting for efficient data mining.
Further studies may include a radiomic analysis to evaluate bone density and its clinical relevance with rib failure.