Pneumonitis after chemoRT and durvalumab: lung damage on CT is confined to the irradiated region
PO-1318
Abstract
Pneumonitis after chemoRT and durvalumab: lung damage on CT is confined to the irradiated region
Authors: Gilles Defraene1, Xander Verbeke2, Saartje Verfaillie2, Patrick Berkovic3, Walter De Wever4, Els Wauters2, Maarten Lambrecht3
1KU Leuven – University of Leuven, Department of Oncology – Laboratory of Experimental Radiotherapy, Leuven, Belgium; 2University Hospitals Leuven, Department of Pneumology, Leuven, Belgium; 3University Hospitals Leuven, Department of Radiation Oncology, Leuven, Belgium; 4University Hospitals Leuven, Department of Radiology, Leuven, Belgium
Show Affiliations
Hide Affiliations
Purpose or Objective
Immune checkpoint inhibitors (ICI) entail an increased risk of pneumonitis when combined with chemo radiotherapy (RT) in locally-advanced non-small cell lung cancer (NSCLC). This often leads to discontinuation of ICI which was shown to affect overall survival. Hence, it is crucial to understand the distinct impact of RT and ICI in order to reduce pneumonitis risk. We therefore quantified and compared lung damage patterns associated with pneumonitis on follow-up CT scans in 3 groups of patients treated with RT alone, ICI alone or RT+ICI combination.
Material and Methods
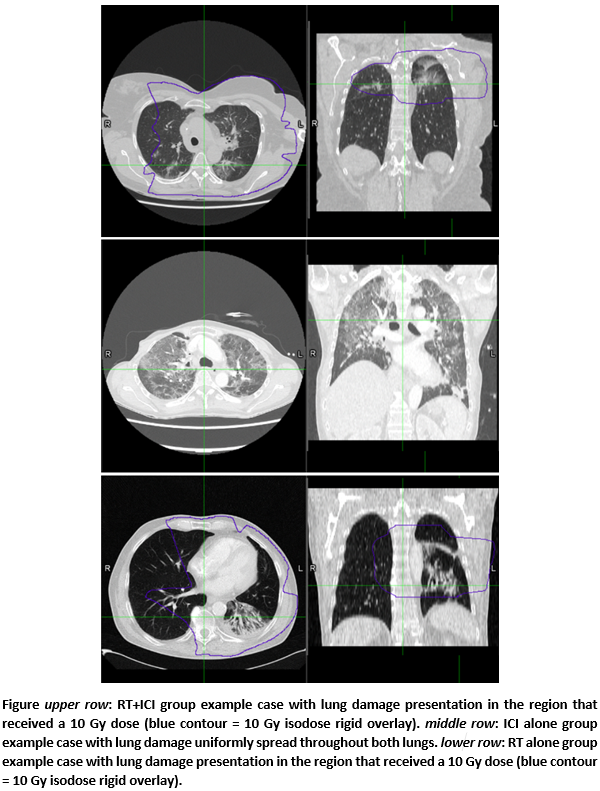
This retrospective study included patients with a clinico-radiological diagnosis of pneumonitis following treatment with RT alone (stage III NSCLC, 55-70 Gy/2-2.75 Gy with 3DCRT or IMRT), ICI alone (stage IV NSCLC, pembrolizumab) or RT+ICI combination (stage III NSCLC, 55-66 Gy/2-2.75 Gy with IMRT + durvalumab) in 2011-2021. Previous irradiation in the thorax region was an exclusion criterion. Planning CTs and dose distributions were rigidly registered to the first follow-up CT with pneumonitis (Figure). Lungs minus GTV contours were manually corrected on the latter (MIM Software). Three first-order CT features were calculated as objective lung damage surrogates: Entropy (ENT) of the lung density distribution, 95% quantile of the density histogram (Q95) and median voxel density. For the groups receiving RT, features were calculated separately for the lung region receiving >10 Gy (L>10Gy), a cut-off based on previous lung damage work, and for the lung region receiving lower doses (L<10Gy). Differences in feature values were assessed by Wilcoxon signed rank tests between lung regions of the same patient and by Mann Whitney U tests between treatment groups.
Results
Thirty-six patients (12 per treatment group) were included with a CT median follow-up time of 3.8 months after RT end (or after pembrolizumab start). Differences in feature values between L>10Gy and L<10Gy were highly significant in the RT+ICI group (p<0.001) and in the RT alone group (p<0.01). These differences were more pronounced for ICI+RT than for RT alone: for L>10Gy ENT=6.49 and ENT=6.23 on average for both groups respectively (p<0.001) while for L<10Gy this was ENT=6.11 and ENT=6.00 (p=0.11). The ICI alone group had similar feature values as in the L>10Gy of RT+ICI (all p>0.05) and these increased feature values were spread throughout the lungs, e.g. average Q95 of -260 HU and -278 HU for left and right lungs (p=0.81). Finally, ICI alone features were significantly different from the L<10Gy of RT+ICI (p<0.02) and RT alone (p<0.02).
Conclusion
Quantitative image features of pneumonitis suggest an increased lung damage inside the 10 Gy isodose region but not outside of this region, when RT is combined with adjuvant durvalumab. In contrast to ICI alone-induced pneumonitis, RT+ICI pneumonitis remains a local problem warranting further research on optimization strategies of low-to-intermediate lung doses by avoidance planning or proton therapy.