Ultra-hypofractionated breast radiotherapy & simultaneous integrated boost for early breast cancer
PO-1275
Abstract
Ultra-hypofractionated breast radiotherapy & simultaneous integrated boost for early breast cancer
Authors: Angel Montero1, Carmen Cañadillas1, Raquel Ciervide1, Mariola Garcia-Aranda1, Beatriz Alvarez1, Alejandro Prado2, Xin Chen-Zhao1, Jeannette Valero1, Mercedes Lopez1, Rosa Alonso1, Ovidio Hernando1, Emilio Sanchez3, Juan Garcia2, Karla Rossi1, Marta Izquierdo1, Pedro Fernandez-Leton2, Carmen Rubio1
1HM Hospitales, Radiation Oncology, Madrid, Spain; 2HM Hospitales, Medical Physics, Madrid, Spain; 3HM Hospitales , Radiation Oncology, Madrid, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
Whole-breast irradiation (WBI) after breast conserving surgery (BCS) is indicated to improve loco-regional control and survival. Former studies showed that addition of tumor bed boost in all age groups significantly improved local control with no apparent impact on overall survival but with an increased risk of worse cosmetic outcome.
Shortened regimens in 3 weeks are considered the standard but recent studies have shown the non-inferiority of 5 fractions in one-week in both locoregional control and toxicity profile. We present our preliminary results of tolerance of ultra-hypofractionated (UHF) in one week WBI schedule with simultaneous integrated boost (SIB) in early breast cancer.
Material and Methods
From March-2020 to March-2022, 383 patients with a median age of 56 years (range 30-99) were treated according to our institution UHF radiotherapy schedule after BCS. Clinical staging (AJCC): Tis 77p (20%), T1a 26p (7%), T1b 87p (22%), T1c 163p (43%), T2 29p (8%). All patients were pN0
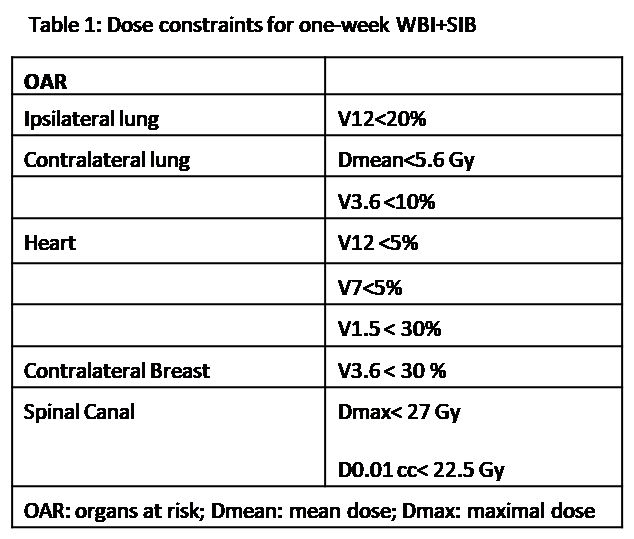
Radiotherapy comprises WBI at 26Gy@5.2Gy/day with a SIB to all patients up to a total dose of 29Gy@5.8Gy/day in 272p (71%), 30Gy@6Gy/day in 100p (26%) and 31Gy@6.2Gy/day in 11p (3%) depending upon margin status. WBI+SIB was delivered by conformal 3-D technique in 366p (96%), VMAT in 16p (4%). Four patients (1%) underwent radiation treatment with deep inspiration breath hold (DIBH). Treatment beam arrangement for SIB comprised of coplanar 2 beams in 2p (0.5%), 3 beams in 142p (37%), 4 beams in 194p (51%), 5 beams in 25p (7%), 9 beams in 1p (0.2%) and 2 arcs in 11p (3%). Median PTV breast volume (mPTVbreast) 725cm3 (114-2409cm3); median PTV boost volume (mPTVboost) 28 cm3 (4.6-198cm3). Dose constraints are detailed in table 1
Systemic therapy: 355p (93%) received hormone therapy and 43p (11%) systemic or targeted chemotherapy.
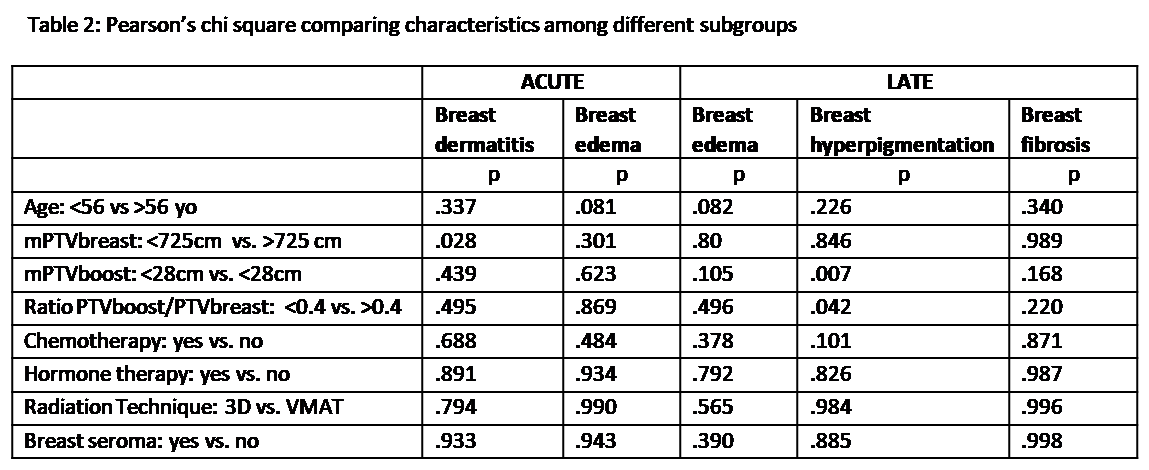
Acute and late toxicities were evaluated according to RTOG/EORTC criteria. Pearson’s Chi square test was used to compare characteristics among different subgroups and statistical significance was considered when reaching a p value <0.05.
Results
With a median follow-up of 18 months (range7-31), all patients are alive without evidence of local, regional or distant relapse.
Acute tolerance: 182p (48%) developed skin toxicity grade 1 and 15p (4%) grade 2; breast edema G1 in 9p (2%), G2 in 2p (0.5%). No other acute toxicities were observed.
Late complications: G1 breast edema in 6p (2%); G1 hyperpigmentation in 20p (5%); G1 late fibroses in 10p (3%) and G2 in 2p (0.5%)
We found a statistically significant correlation between the mPTVbreast and presence of skin toxicity (p =0.028) as well as a significant correlation between late hyperpigmentation with the mPTVboost (p = 0.007) and the ratio PTV boost volume/PTV breast volume (p = 0.042) (Table 2).
Conclusion
UHF-WBI with SIB in 5 fractions along one-week is feasible and well tolerated. Higher boost volumes are associated with a slightly worse long-term cosmetic outcome. However, longer follow-up is necessary to confirm these results.