Simultaneous integrated boost within the lymphatic drainage system in breast cancer
PO-1274
Abstract
Simultaneous integrated boost within the lymphatic drainage system in breast cancer
Authors: Antonia Peiler1, Sophie T. Klusen1, Rebecca Asadpour1, Stephanie E. Combs1,2,3, Kai J. Borm1
1Technical University Munich, Medical School, Klinikum rechts der Isar, Department of Radiation Oncology, Munich, Germany; 2Deutsches Konsortium für translationale Krebsforschung (DKTK) , Partner Site Munich, Munich, Germany; 3Institute of Radiation Medicine, Helmholtzzentrum München, Munich, Germany
Show Affiliations
Hide Affiliations
Purpose or Objective
There has been a progressive de-escalation of axillary surgical therapy within the framework of breast cancer treatment due to the questionable oncological benefit and the associated toxicity of axillary lymph node dissection. Together with the improving resolution of diagnostic imaging, morphologically abnormal lymph nodes can be detected more frequently. In lymph-node positive patients, locoregional treatment of the lymph node drainage system has the potential to improve the oncological outcome. If resection of the remaining suspect lymph nodes is not feasible, a simultaneous boost to the lymph node metastases (LN-SIB) can be applied. We aim to provide preliminary data on the outcome and safety of this technique as there is no data on this yet.
Material and Methods
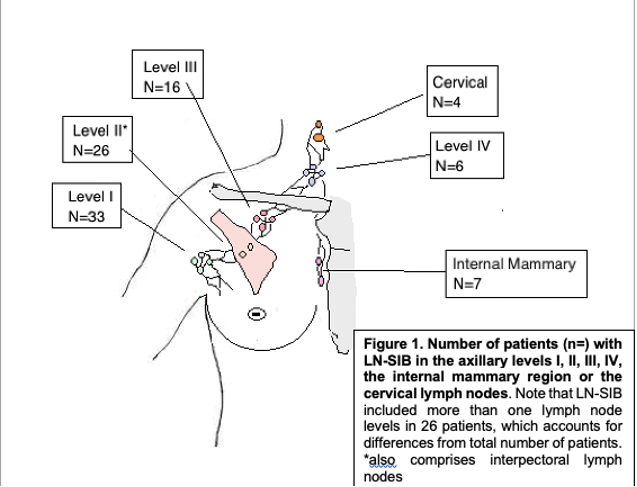
48 breast cancer patients with remaining suspect lymph nodes after surgery who received adjuvant radiotherapy of the chest/chest wall (50.4 Gy in 28 fractions) and an integrated boost within the lymph node system (median dose: 58.8 Gy / 2.1 Gy (range 56-63 Gy / 2-2.25 Gy)) were included in the current study (2010-2020 at TU München). The treatment decisions were discussed interdisciplinary with consideration of another individual surgical intervention before consensus of radiotherapy. The brachial plexus was contoured in every case and the dose within the plexus PRV (+0.3-0.5mm) was limited to an EQD2 of 59 Gy.
All patients received structured radio-oncological and gynecological follow-up (FU) by clinically experienced physicians. Intervals for radio-oncological FU were at 0 weeks, 6 weeks, 3 months, 6 months and subsequent annually after irradiation.
Results
The median FU time was 557 days (82.4 weeks) and ranged from 41 to 3373 days.
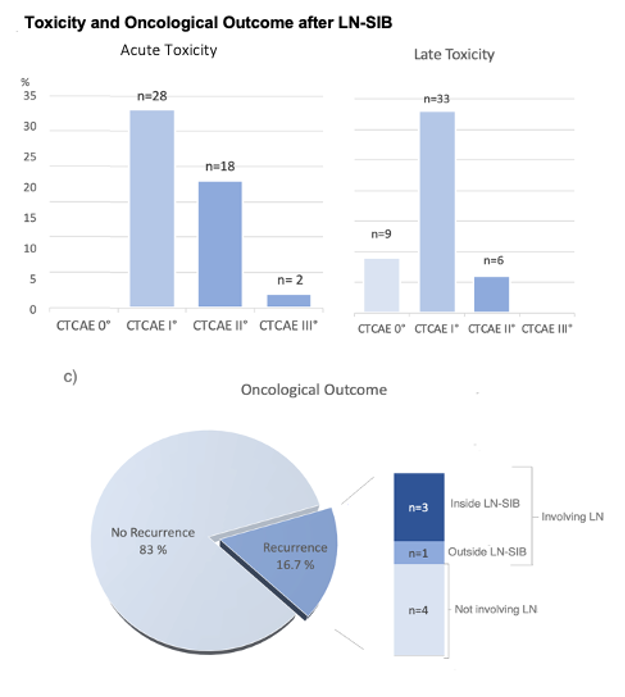
Overall, 28 patients developed I°, 18 patients II° and 2 patients III° acute toxicity.
There were no severe late side effects (≥ III°) observed during the follow-up period. The most frequent chronic side effect was fatigue. One patient (2.1 %) developed pain and mild paresthesia in the ipsilateral arm indicating brachial plexopathy
After a FU of 557 days (41 to 3373 days), in 8 patients a recurrence was observed (16.7%). In 4 patients the recurrence involved the regional lymph node system. Hence, local control after a median FU of 557 days was seen in 44 patients (91.6 %).
Conclusion
Our analyses indicate a predominantly low to moderate acute or late toxicity after LN-SIB and reasonable locoregional control. LN-SIB-irradiation may be considered as a potential treatment option if re-resection of residual lymph nodes after initial surgery is not feasible. Patients receiving a LN-SIB must be informed about a higher risk of brachial plexopathy, especially if a large volume is included in the LN-SIB.