Risk stratification for internal mammary lymph node irradiation based on dynamic MRI vessel imaging
Sophie Therese Klusen,
Germany
PO-1264
Abstract
Risk stratification for internal mammary lymph node irradiation based on dynamic MRI vessel imaging
Authors: Sophie Klusen1, Rebecca Asadpour1, Eva Maria Fallenberg2, Stephanie Elisabeth Combs1,3, Kai Joachim Borm1
1Technical University Munich, Radiation Oncology, Munich, Germany; 2Technical University Munich, Radiology, Munich, Germany; 3Helmholtz Zentrum Munich, Innovative Radiotherapy and Radiation Science, Munich, Germany
Show Affiliations
Hide Affiliations
Purpose or Objective
Irradiation of the lymphatic system is associated with improved distant metastasis free- and overall survival in high-risk breast cancer. However, inclusion of the internal mammary region in the target volume markedly increases the dose to the heart. Estimating the individual risk of subclinical involvement of the internal mammary lymph node (IMN) allows the potential benefit of (full) IMN irradiation to be weighed against potential cardiac side effects. In the current study we aim to investigate whether location of the tumor and feeding vessels closed to the internal mammary perforator vessels (IMPV) in dynamic contrast enhanced MRI images (DE-MRI) can be considered a risk factor for IMN involvement.
Material and Methods
We examined retrospectively 86 sets of pre-treatment DE-MRI-scans of breast cancer patients with ipsilateral clinically pathological lymph nodes in the axilla, of which 43 patients had positive and 43 negative IMN. Based on maximum intensity projection (MIP) of DE-MRI we assessed whether the tumor has contact to the IMPV. If there was contact between tumor and IMPV we differentiated between contact to a “main IMPV” or smaller “side branches”.
Results
38 of 86 tumors (44.2%) were located in the right breast, 46 tumors (53.5%) in the left breast. The tumor location was in 16.3% (7/43) medial, 30.2% (13/43) central, 32.6% (14/43) lateral and 20.9% (9/43) multicentric in patients with positive IMN and 4.7% (2/43) medial, 20.9% (9/43) central, 34.9% (15/43) lateral and 39.5% (17/43) multicentric in patients with negative IMN.
In patients with positive IMN, 100 % of tumors had contact with IMPV: In 36 cases (83.7%) to a main branch and in 7 cases (16.3%) to IMPV side branches.
In patients without pathological IMN on the other hand, still in 81.4 % of cases the tumor had contact to IMPV, however only in 13 patients (30.2 %) there was contact between tumor and IMPV main branches.
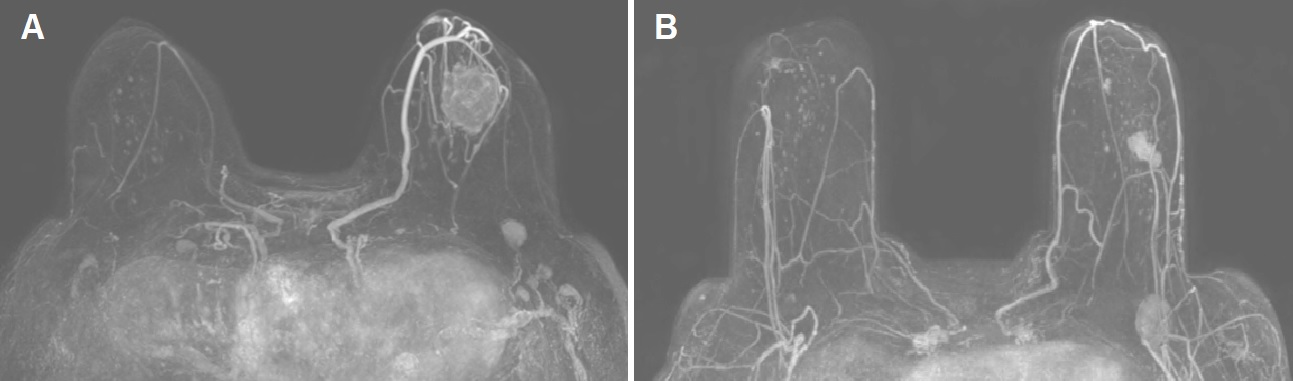
A Tumor with contact to main branch of IMPV in patient with positive IMN
B Tumor without contact to IMPV in patient with negative IMN
Conclusion
38 of 86 tumors (44.2%) were located in the right breast, 46 tumors (53.5%) in the left breast. The tumor location was in 16.3% (7/43) medial, 30.2% (13/43) central, 32.6% (14/43) lateral and 20.9% (9/43) multicentric in patients with positive IMN and 4.7% (2/43) medial, 20.9% (9/43) central, 34.9% (15/43) lateral and 39.5% (17/43) multicentric in patients with negative IMN.
In patients with positive IMN, 100 % of tumors had contact with IMPV: In 36 cases (83.7%) to a main branch and in 7 cases (16.3%) to IMPV side branches.
In patients without pathological IMN on the other hand, still in 81.4 % of cases the tumor had contact to IMPV, however only in 13 patients (30.2 %) there was contact between tumor and IMPV main branches.