Axillary lymph nodes incidental dose with standard 3D-CRT: a retrospective evaluation
PO-1257
Abstract
Axillary lymph nodes incidental dose with standard 3D-CRT: a retrospective evaluation
Authors: Marzia Borgia1, Consuelo Rosa1, Fiorella Cristina Di Guglielmo1, Lucia Anna Ursini1, Marianna Nuzzo1, Luciana Caravatta1, Domenico Genovesi1
1"SS Annunziata" Hospital, "G. D'Annunzio" University, Radiation Oncology Unit, Chieti, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
In the past, axillary lymph node dissection (ALND) represented the preferred treatment in patients with clinically negative axilla and positive sentinel lymph node biopsy (SLNB), completing tumour staging and providing local control (LC). ACOSOG Z0011, comparing cN0 patients with positive SLNB treated with or without ALND, showed ALND safely omission, leading to focus on incidental dose to the axilla that was assumed to eradicate additional unseen axillary lymph nodes metastases. Nevertheless, the correlation between the adequate coverage of theincidental dose to the axilla, remains debated. We aim to evaluate the incidental dose to axillary levels I and II in patients with positive SLNB not submitted to ALND.
Material and Methods
We retrospective analyzed breast cancer patients treated in our Center. We included patients undergone to breast conservative surgery without ALND and treated with conventional fractionated 3D-CRT without a prescription of intentional axillary irradiation. A retrospective delineation of axillary level I (L1) and axillary level II (L2) was performed according to ESTRO contouring guidelines. A dosimetric evaluation was conducted. Clinical outcomes as overall survival (OS), disease-free survival (DFS) and LC were analysed, measured from surgery until the first event.
Results
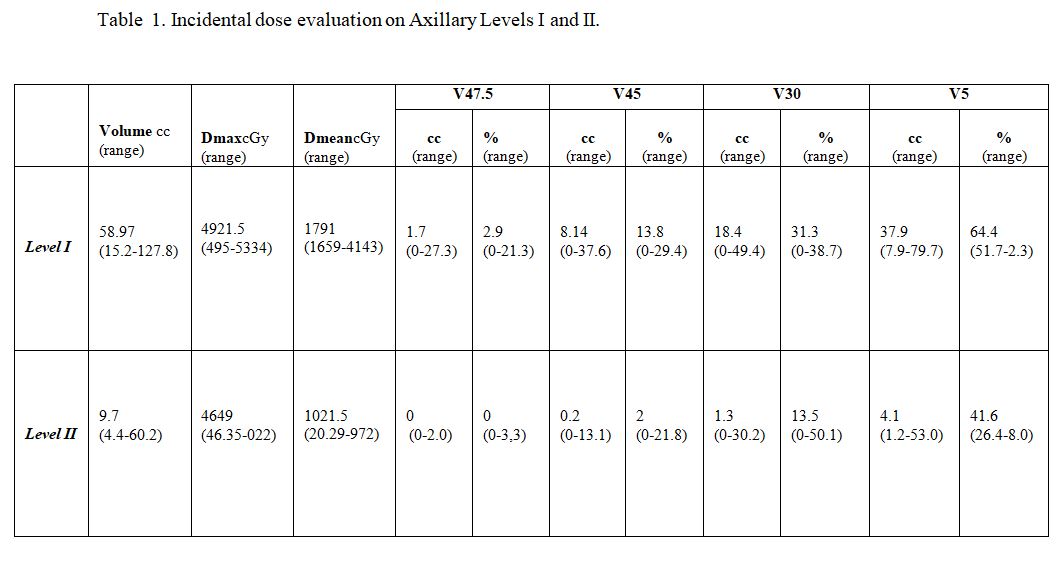
Fifty-two patients, undergone to conservative surgery and SLNB with pN1, were analyzed. Median age was 58 years (range=38-73 years). Dosimetric values were reported in table 1. The mean breast PTV was 748.6 cc (range=218.1-1287,9cc) with a median maximal dose of 5328 cGy (range= 5258-5428 cGy) and a median mean dose of 5000 cGy (5000-5073 cGy). The mean L1 and L2 volume were 58.97 cc (range=15.2-127.8 cc) and 9.7 cc (range=4.4-60.2 cc) respectively. For L1, the median maximal and mean doses were 4921.5 cGy (range= 495-5334 cGy) and 1791 cGy (1659-4143 cGy) respectively. For L2, the median maximal and mean doses were 4649 cGy (range= 46.35-5022 cGy) and 1021cGy (range= 20.29-2972 cGy), respectively. The median follow up was 52.7 months (13.8-87.4 months). The 4-year OS, DFS and LC were 100%, 88.5% and 94.2% respectively. No patient had complete coverage of L1 and L2 as assumed by the median V47.5Gy and V45Gy coverage.
Conclusion
In this study, incidental dose to axillary levels with 3D-CRT, did not delivered a therapeutic dose to L1 and L2. When required, definitive irradiation of the L1 and L2 needs a modification of standard tangential fields and the targeting of axillary lymph node volumes, in addition to the breast gland volumes.