Implementation of the 1.5T MR-linac: healthy volunteers, screen recording and initial experience
PO-1076
Abstract
Implementation of the 1.5T MR-linac: healthy volunteers, screen recording and initial experience
Authors: Madeline Michel1, Zelda Paquier2, Hamza Alghamdi1, Christelle Bouchart1, Christine Collen1, Akos Gulyban2, Philippe Martinive1, Nick Reynaert2, Dirk Van Gestel1, Robbe Van den Begin1
1Institut Jules Bordet, Radiation oncology, Brussels, Belgium; 2Institut Jules Bordet, Medical Physics, Brussels, Belgium
Show Affiliations
Hide Affiliations
Purpose or Objective
Adaptive radiotherapy has seen a major breakthrough thanks to the advent of MR-guided radiotherapy. Here, we aim to evaluate the role of healthy volunteers, a video capture system and self-training towards the GoLive with a 1.5T MR-Linac. Additionally we report our initial experience in terms of treatment time, choice of adaptation and adjustments of the clinical workflow.
Material and Methods
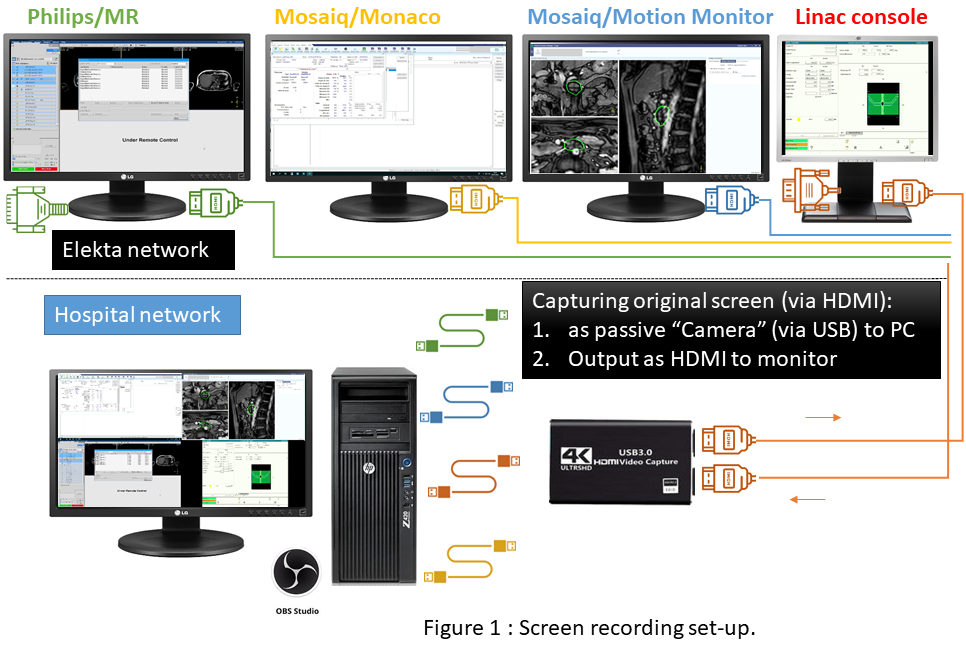
The clinical readiness period of the MR-Linac Unity (Elekta Ltd, Stockholm, Sweden) started in March 2022, following the official trainings. Our self-preparation consisted of 1) establishing a preparation procedure, 2) inviting healthy volunteers to test the MR-Linac workflow (without actual irradiation), 3) installing a screen recording system of four consoles simultaneously for off-line analysis (fig.1), 4) performing end-to-end and treatment interruption tests using the Zeus moving phantom (CIRS, Norfolk, VA, USA). GoLive was successful in June 2022. For each treatment session, the screen recordings were analyzed to determine the duration of MRI acquisition, evaluation, contour adaptation, treatment planning, beam-on time, and determine the time until proper decision in case of problem troubleshooting. Additionally a weekly briefing meeting was organized to discuss and improve our workflow.
Results
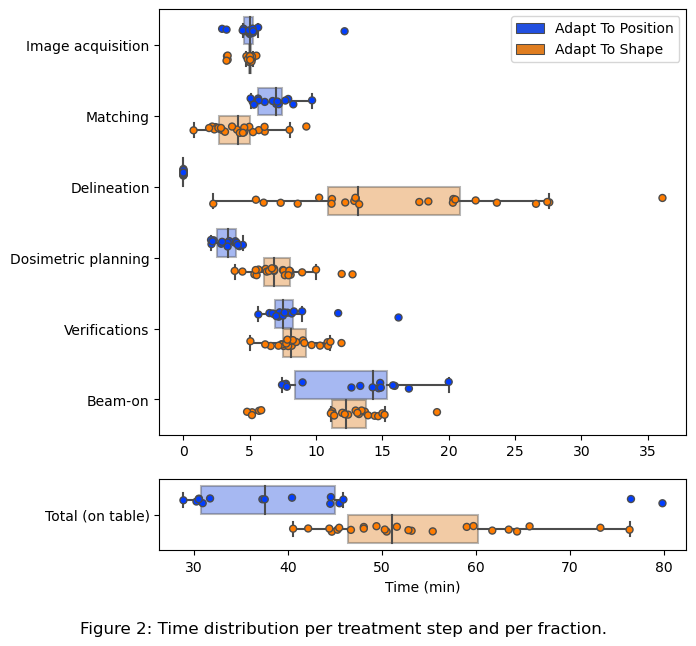
During the GoLive preparation a total of 26 volunteers were scanned: 12 pelvis, 2 brain, 5 abdomen, 4 thorax, 3 head and neck, providing sufficient information about expected image quality, preferred acquisitions and familiarization with the machine and workflow. Screen recording became essential for timing and troubleshooting. The Zeus phantom was used for the end-to-end test (including cine MRI) and treatment interruption training. Since the clinical GoLive, a total of eight patients have been treated on the Unity following a hypofractionated 5-session regimen for lymph nodes (6), pancreatic tumour (1) and rectum (1). The patients spent an average of 48.3 minutes (range 28.9 - 76.5) on the treatment table (fig.2). Two patients were treated with adapt-to-position (ATP) only, four with adapt-to-shape (ATS) only, and two patients with a mix of both. ATS sessions lasted on average 12.7 minutes longer than ATP. All patients tolerated the treatments well. Two fractions out of forty were not completed as planned: one required a plan completion in the same day due to a machine problem, while the other required one day of delay because of a software connectivity issue. Weekly briefing meetings resulted in the development of a patient-specific “briefing sheet” to summarize the acquisition protocol (including functional sequences), contouring strategy and plan optimization particularities, to allow smooth communication among staff.
Conclusion
Healthy volunteers and the Zeus phantom played a pivotal role in the preparation to GoLive with the Unity MR-Linac, especially combinined with screen capturing and off-line analysis. Weekly briefing meetings are warranted to optimize the online adaptive workflow.