Older men’s experience of sexual dysfunction associated with prostate cancer
William Kinnaird,
United Kingdom
PO-1061
Abstract
Older men’s experience of sexual dysfunction associated with prostate cancer
Authors: William Kinnaird1, Michael Kirby2, Patricia Schartau3, Valerie Jenkins4, Stephen Allen5, Heather Payne6
1University College London Hospitals, Radiotherapy, London, United Kingdom; 2Trends in Urology and Men's Health, Editor, London, United Kingdom; 3University College London, Primary Care and Population Health, London, United Kingdom; 4University of Brighton, Sussex Health Outcomes Research & Education in Cancer , Brighton, United Kingdom; 5Tackle Prostate, Clinical Advisory Board Member, London, United Kingdom; 6University College London, Medical Physics and Biomedical Engineering, London, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Sexual activity in older adults is associated with a range of physical and psychological health benefits. However, many older people do not access support from healthcare professionals (HCPs) when experiencing sexual health concerns. Almost all prostate cancer (PCa) treatments are associated with sexual problems that can have detrimental effects on overall wellbeing. This study is the first to investigate in depth the impact age has on PCa patient’s experience of sexual dysfunction and accessing support.
Material and Methods
An anonymous online survey was distributed via email, social media and peer-support group networks in collaboration with the charity Prostate Cancer UK. A total of 49 questions focused on PCa patients’ experience of sexual dysfunction and accessing support. Data was analysed by age, with participants split into ‘older men’ aged >75 and ‘younger men’ aged ≤75. The chi-square test was used for categorical variable analysis.
Results
A total of 654 out of 893 adult participants met the inclusion criteria and were included in the analysis. Of those n=85 (13.1%) were aged >75.
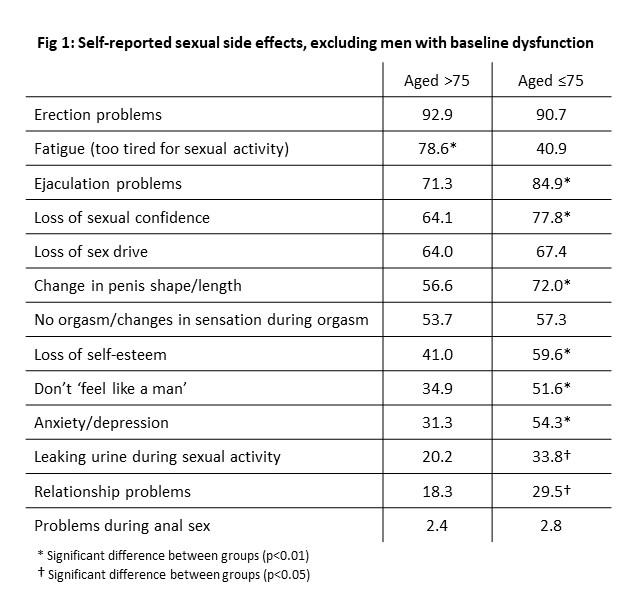
Physical and psychological sexual problems were common among older men, even after those with baseline dysfunction were excluded. The majority reported erection problems, fatigue (too tired for sexual activity), ejaculation problems, loss of sexual confidence, loss of sex drive, change in penis shape/length and no orgasm or changes in sensation during orgasm [Fig.1].
Sexual activity was rated as ‘fairly/very important’ by 62.4% (n=53) of men aged >75. Further, 52.9% (n=45) of older men reported ‘sexual problems’ to be in their top three current concerns, the highest overall ranked concern from a list of 15 options. The comparative figures for younger men were 80.6% and 63.0%.
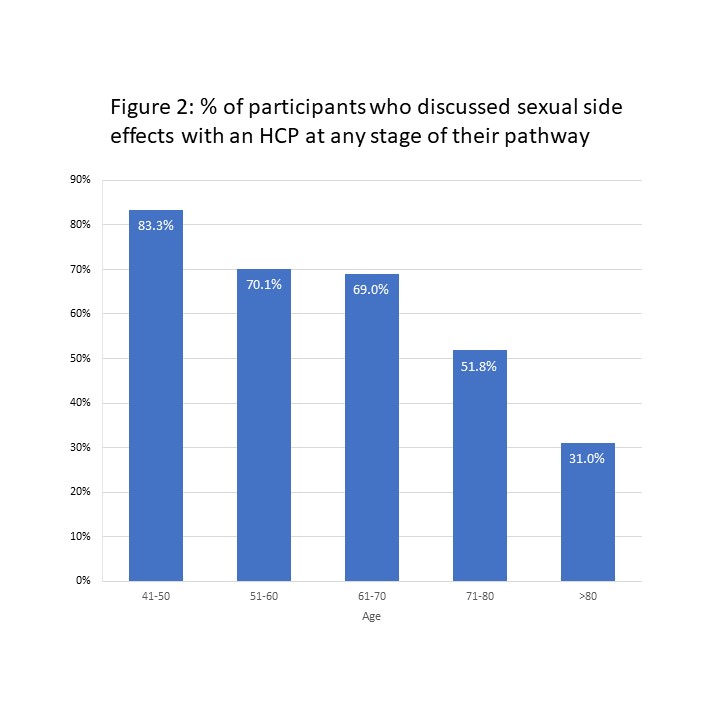
Despite this, older men were significantly less likely to have discussed the sexual side effects of PCa treatment with an HCP at any stage of their treatment (40.0% vs 65.3%, p<.001). The number of men reporting discussions declined as age increased [Fig.2]. Older men who did report discussions of sexual side effects were still less likely to be offered a referral to a specialist clinic at any stage for support than younger men (26.5% vs 43.8%, p=.05).
Just 31% of older men agreed with the statement ‘I was told everything I needed to know about sexual problems’ and only 40% described the support they received as ‘adequate’. The comparative figures for younger men were 33% and 38%.
Conclusion
This study is the first to report in depth on older men’s experience of sexual dysfunction associated with PCa. Findings suggest wide-ranging physical and psychological sexual side effects among men aged >75 are common and distressing. Despite this, older men are less likely to access support through HCPs. The results highlight the importance of giving older men equitable access to information and supportive care. The work forms part of an ongoing project to publish new guidelines aimed at reducing inequalities in sexual dysfunction support.