Lymphopenia during NSCLC ChemoRT is proportional to FLT-detected suppression of irradiated marrow
Michael MacManus,
Australia
MO-0473
Abstract
Lymphopenia during NSCLC ChemoRT is proportional to FLT-detected suppression of irradiated marrow
Authors: Michael MacManus1, Elizabeth Prinz1, Fiona Hegi-Johnson1, Jason Callahan2, Rodney Hicks2, Tim Akhurst2, Sophia Xie3, Sarah Everitt1
1Peter MacCallum Cancer Centre, Radiation Oncology, Melbourne, Australia; 2Peter MacCallum Cancer Centre, Molecular Imaging, Melbourne, Australia; 3Peter MacCallum Cancer Centre, Biostatistics and Clinical Trials, Melbourne, Australia
Show Affiliations
Hide Affiliations
Purpose or Objective
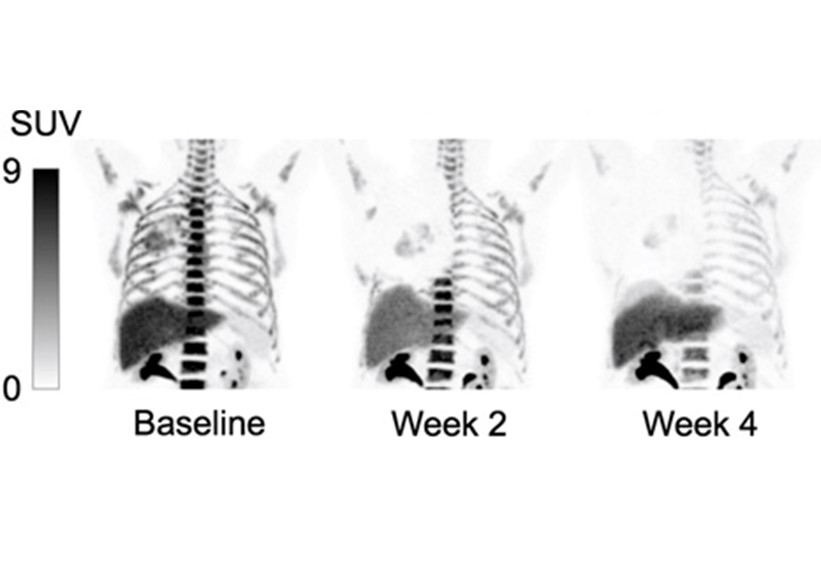
Adjuvant immunotherapy improves survival after chemoradiotherapy (chemoRT) in advanced non-small-cell lung cancer (NSCLC) but immunotherapy requires a functioning immune system. Bone marrow is exquisitely sensitive to radiation and lymphopenia is common after chemoRT. The potential association between loss of proliferating irradiated bone marrow and cytopenias during chemoRT has not been reported in NSCLC. We used serial 18F-fluorothymidine (FLT) PET scans to quantify loss of proliferating bone marrow during chemoRT (upper figure) and correlated bone marrow ablation with changes in circulating lymphocyte counts.
Material and Methods
We conducted a retrospective analysis of FLT-PET scans from a prospective observational trial of serial PET imaging in NSCLC patients treated with chemoRT to 60 Gy. Of 60 enrolled patients, complete data for FLT-PET scans at baseline and weeks 2 and 4 were available for 28. The bony skeleton was auto-segmented in MIM software enabling FLT uptake in bone marrow to be quantified. The percentage of total injected FLT delivered to bone marrow provided a baseline value. Based on quantitative dose response analyses (data reported in a companion abstract), volumes of bone marrow exposed to >3 Gy at weeks 2 and 4 were considered to have no FLT-PET-detectable marrow proliferation. The percentage of the total injected dose of FLT missing from the bone marrow in the volume irradiated to >3 Gy was estimated by comparing 3 Gy isodose volumes at weeks 2 and 4 with the baseline scan. Changes in lymphocyte nadir (lowest value) in periods from baseline to week 2 and baseline to week 4 were analysed. Lymphocyte counts were normalised, assuming the baseline to be 0%. Estimated percentage losses of marrow from baseline to weeks 2 and 4 were correlated with % loss of lymphocyte counts during the same periods.
Results
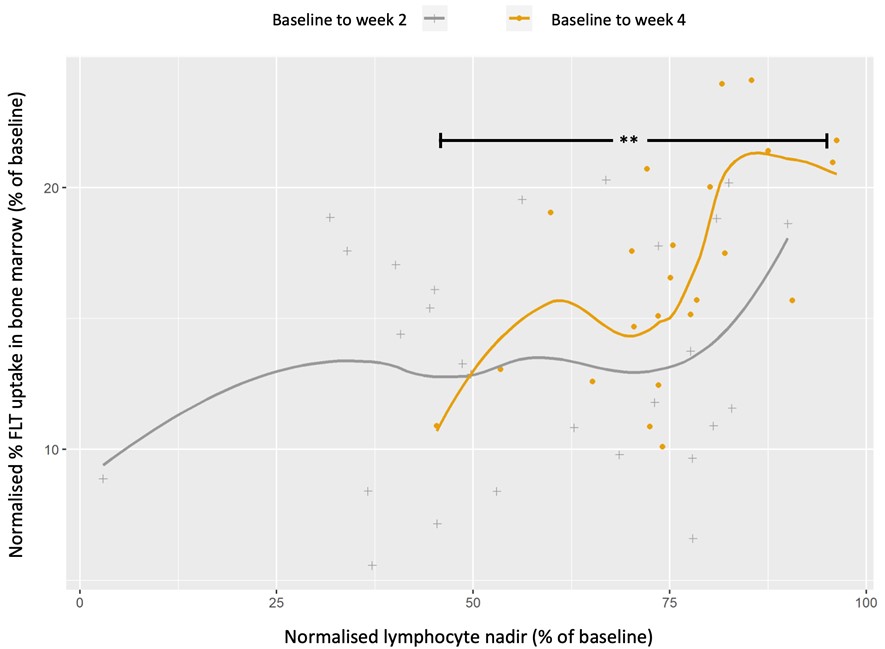
A scatter plot of % loss of bone marrow vs % change in lymphocyte counts at weeks 2 and 4 was produced (lower figure). The % loss of FLT uptake in bone marrow and reductions in lymphocyte counts were positively correlated from baseline to both weeks 2 and 4. The correlation from baseline to week 4 was highly significant (p<0.003). The correlation from baseline to week 2 was comparatively weaker, suggesting that time is required for radiation damage to be fully expressed.
Conclusion
There was a strong correlation between the estimated percentage of proliferating bone marrow ablated by radiation and percentage worsening of lymphocyte nadirs from baseline to week 4. Relationships between percent marrow ablation and lymphocyte counts were non-linear suggesting that other factors may contribute.