Impact of gross vascular invasion on NSCLC outcomes: propensity matched cohort analysis
Atazhan Ushkempirov,
Kazakhstan
MO-0468
Abstract
Impact of gross vascular invasion on NSCLC outcomes: propensity matched cohort analysis
Authors: Atazhan Ushkempirov1, Corinne Faivre-Finn1, Gareth Price1, Ahmed Salem2
1University of Manchester, Faculty of Biology, Medicine and Health, Manchester, United Kingdom; 2Hashemite University, Faculty of Medicine, Zarqa, Jordan
Show Affiliations
Hide Affiliations
Purpose or Objective
Gross vascular invasion is reported to be associated with a higher risk of severe toxicity and premature death in non-small cell lung cancer (NSCLC) patients treated with radiotherapy. We investigated the association between the presence, location and grade of gross vascular invasion with survival and post-radiotherapy haemorrhage.
Material and Methods
Patients with T4N0-3M0 NSCLC treated with curative-intent radiotherapy (dose ≥40Gy) ±chemotherapy at the Christie NHS Foundation Trust (Manchester, UK) were retrospectively reviewed. Gross vascular invasion was defined based on a prospective review of chest CT and/or PET/CT and graded as per Han et al. IJROBP. 2014. The association between gross vascular invasion and post-treatment haemorrhage was investigated using Fisher’s exact test. Univariable and multivariable analyses were conducted to investigate the association of the following covariates with overall survival at 2-years: age, gender, histological subtype, gross tumour volume, nodal staging, ECOG performance score and the presence, location and grade of gross vascular invasion. Two comparison cohorts were propensity score matched by a 1:1 ratio using the following covariates: ECOG performance score, sex, age and histological subtype.
Results
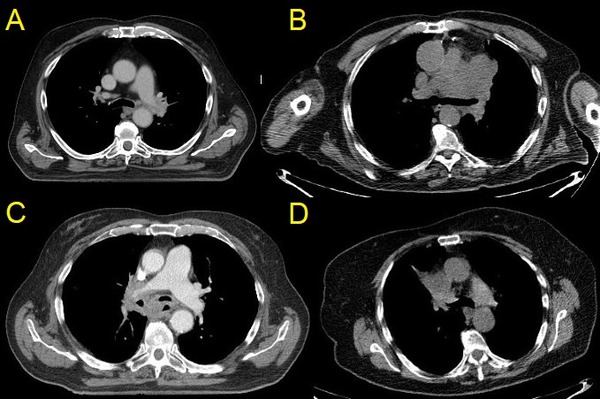
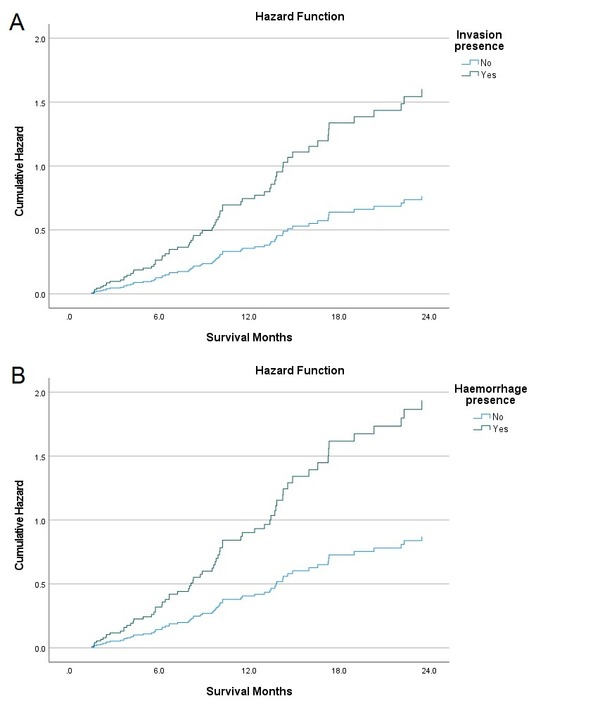
Of 370 patients reviewed, 50 (13.5%) demonstrated gross vascular invasion. Only 3 great vessels were invaded: left (N=28) and right pulmonary artery (N=9), superior vena cava (N=8) and both right pulmonary artery and superior vena cava (N=5). Grade 4 gross vascular invasion (slit-like narrowing) was seen in N=40 (80%) while grade 5 (encasement with extensive invasion) was seen in N=10 (20%); figure 1. These patients were matched with a NSCLC cohort who did not exhibit gross vascular invasion (N=50). Post-radiotherapy grade 4-5 haemorrhage occurred in 5 (10%) in the gross vascular invasion cohort and in 2 (4%) patients in the control cohort. Fisher’s exact tests did not reveal any association between the presence, location and grade of gross vascular invasion and post-radiotherapy haemorrhage occurrence and grading (P>0.05). Multivariable analysis revealed that age, ECOG performance score and histological subtype were significantly associated with 2-year overall survival (P<0.05). The presence of gross vascular invasion and post-treatment haemorrhage were associated with numerically worse 2-year overall survival, but this was not statistically significant (HR 2.09, P=0.101 and HR 2.22, P=0.096, respectively); Figure 2.
Conclusion
In this propensity-matched cohort analysis of NSCLC patients treated with radiotherapy, we found no statistically significant association between the presence, location and grade of gross vascular invasion with either post-treatment haemorrhage or worse 2-year overall survival. Our findings could be relevant to the design of future studies and clinical practice.