Markerless MRI-only workflow for primary prostate radiotherapy
MO-0387
Abstract
Markerless MRI-only workflow for primary prostate radiotherapy
Authors: Monica Buijs1, Nikki de Munk1, Steven Takken1, Peter Remeijer1, Uulke van der Heide2
1NKI-AvL, Radiation Oncology, Amsterdam, The Netherlands; 2NKI-AvL, Radiation Oncolgy, Amsterdam, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Currently it is a challenge to visualize markers on a MRI synthetic CT scan (sCT) and subsequently to perform a marker-based MRI-only image-guided radiotherapy (IGRT) workflow for primary prostate cancer radiotherapy. As improvements in Cone beam CT image quality allowed the introduction of soft tissue based IGRT for prostate and nodal RT, the aim of this study was to assess the feasibility of implementing a markerless MRI-only IGRT workflow for primary prostate RT.
Material and Methods
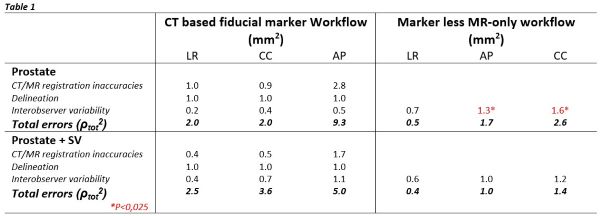
To assess the feasibility of a markerless MRI-only workflow, without increasing treatment margins, typical workflow-related geometrical uncertainties of a CT- and MRI-only based workflow were compared.
The following geometrical uncertainties are relevant in a CT-based workflow:
- The CT to MRI registration related inaccuracies, calculated as the systematic difference in soft tissue and fiducial marker based prostate registration results in the LR,CC and AP direction for 19 prostate patients.
- The systematic delineation error due to adapting the MRI based delineation to the anatomy on the CT, estimated to be ~1 mm by reviewing the adapted delineations in the same patient group in collaboration with a radiation oncologist.
- The calculated Root Means Square of the interobserver variability (IOV) calculated for marker based CBCT to CT registrations, performed by 5 observers on 5 CBCTs of 10 patients treated on the prostate solely and for 10 patients treated on the prostate and seminal vesicles.
In a markerless MR-only workflow a CT scan is no longer required, subsequently removing the CT-MRI registration and delineation uncertainties, therefore the only remaining uncertainty is the IOV, calculated for soft tissue-based CBCT to sCT registrations, again performed by 5 observers on 5 CBCTs of 10 patients with prostate only and in 10 patients with prostate and the seminal vesicles as target volume.
The IOV was statistically compared with a one-sided Levene’s test using a p-value of 0,025 assuming the IOV to be larger for soft tissue registration compared to marker registration.
Results
In table 1 the workflow-related uncertainties are summarized. For the patients, treated solely on the prostate, the IOV increased ~1 mm in the CC and AP direction for soft tissue registration compared to marker registration, which was found to be significant (P<0,025). For patients treated on the prostate and seminal vesicles, the IOV was not significantly different. The total quadratic sum of the workflow related geometrical uncertainties was smaller in case of the markerless MR-only workflow.
Conclusion
The removal of the CT-MRI related delineation and registration uncertainties in an MRI-only workflow outweighs the slight increase in IOV related to performing soft tissue registration instead of marker registration in the IGRT procedure. Therefore, the implementation of a markerless MR-only workflow is considered to be feasible for primary prostate patients.