Risk factors associated with acute skin toxicities in patients treated with Proton Beam Therapy
Simona Gaito,
United Kingdom
MO-0383
Abstract
Risk factors associated with acute skin toxicities in patients treated with Proton Beam Therapy
Authors: Kenneth Oguejiofor1, Simona Gaito2, Anna France2, Shermaine Pan2, Marianne Aznar3, Peter Sitch2, Michael Merchant4, Ed Smith2, Jenny Richardson2
1Christie Hospital Manchester, Proton Beam Therapy Centre , Manchester, United Kingdom; 2Christie Hospital Manchester, Proton Beam Therapy Centre, Manchester, United Kingdom; 3University of Manchester / Christie Hospital Manchester, Radiotherapy-Related Research Group, Manchester, United Kingdom; 4University of Manchester / Christie Hospital Manchester, PRECISE group, Manchester , United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Acute radiotherapy induced skin toxicities (RIST) are reported to be higher in patients treated with proton beam therapy (PBT) due to loss of the build-up effect. Predictive factors of acute RIST in patients treated with PBT remains largely undefined. In this study, we retrospectively reviewed the acute RIST of patients treated with PBT to identify dose and volume thresholds predictive of acute RIST.
Material and Methods
Patients treated with pencil beam scanning (PBS) at a National PBT centre between December 2018 to October 2022, who developed Grade 0 (G0) or Grade 2+ (G2+) acute RIST were included in this study. Anonymised demographic and clinical data were obtained retrospectively from electronic patient records. Dosimetric data required manual extraction from Eclipse v16.1.
Skin structure is defined as 5mm rind grown as an inner margin from the patient contour. The following skin dose–volume statistics were collected: Dmax (maximum dose to any pixel inside the skin contour) and dose to skin volumes (cm3) in 5Gy increments (V5Gy, V10Gy etc). The RTOG criteria was used in grading acute RIST. Preliminary analyses of dosimetric data of patients with G0 vs G2+ acute RIST are presented, with significance assessed at the 5% level using t-tests and univariate logistic regression models, and risk thresholds found using receiver operating characteristic (ROC) curves.
Results
Of 893 patients treated with PBS PBT, 171 had G0 RIST and 342 had G2+ RIST. So far, of these, 191 patients have had their dosimetric information extracted for inclusion in the study, 46 G0 and 145 G2+ RIST. Of these 191 patients, the three major indications for PBT were head and neck (20%), sarcoma (28%) and chordoma (16%). The median age of patients treated was 18 years (1 – 82), with 42% paediatric (<16Y), 17% teenage and young adult (16-24Y) and 41% adults (25Y+).
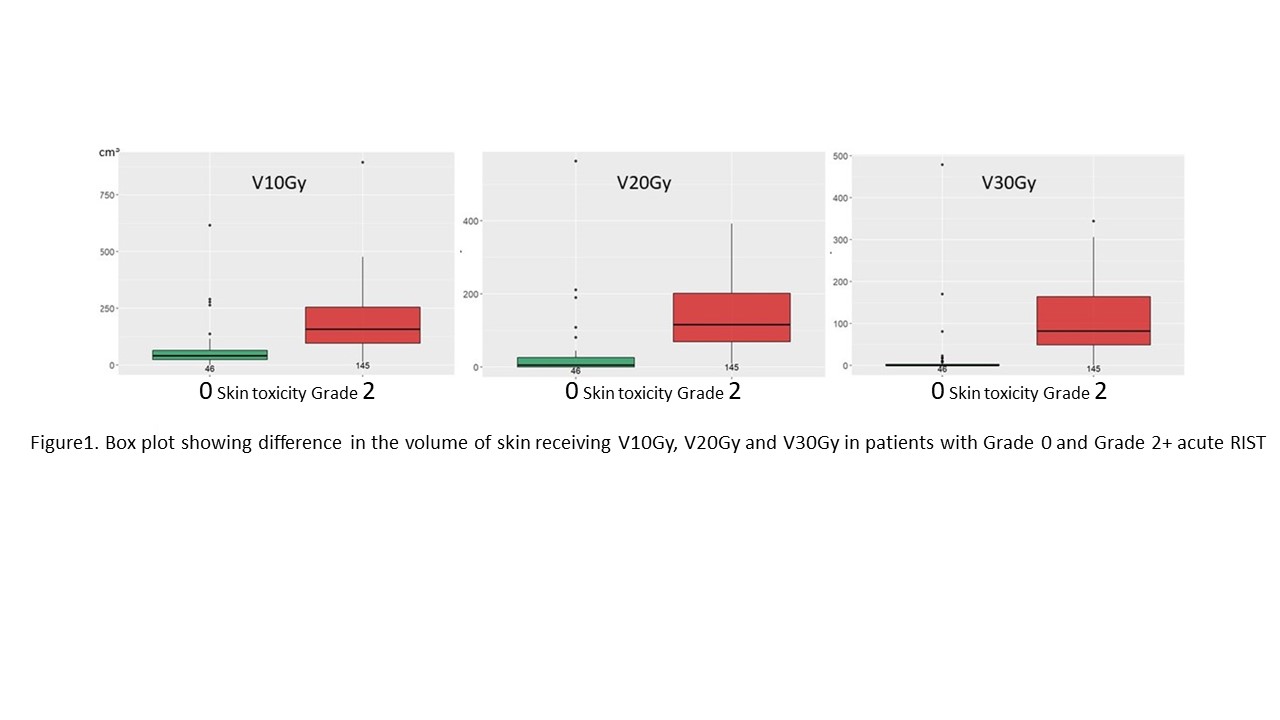
For patients who developed acute RIST of G2+, the median volume receiving 10Gy, 20Gy and 30Gy were significantly higher (P<0.0001) than in those without acute RIST, (Figure 1).
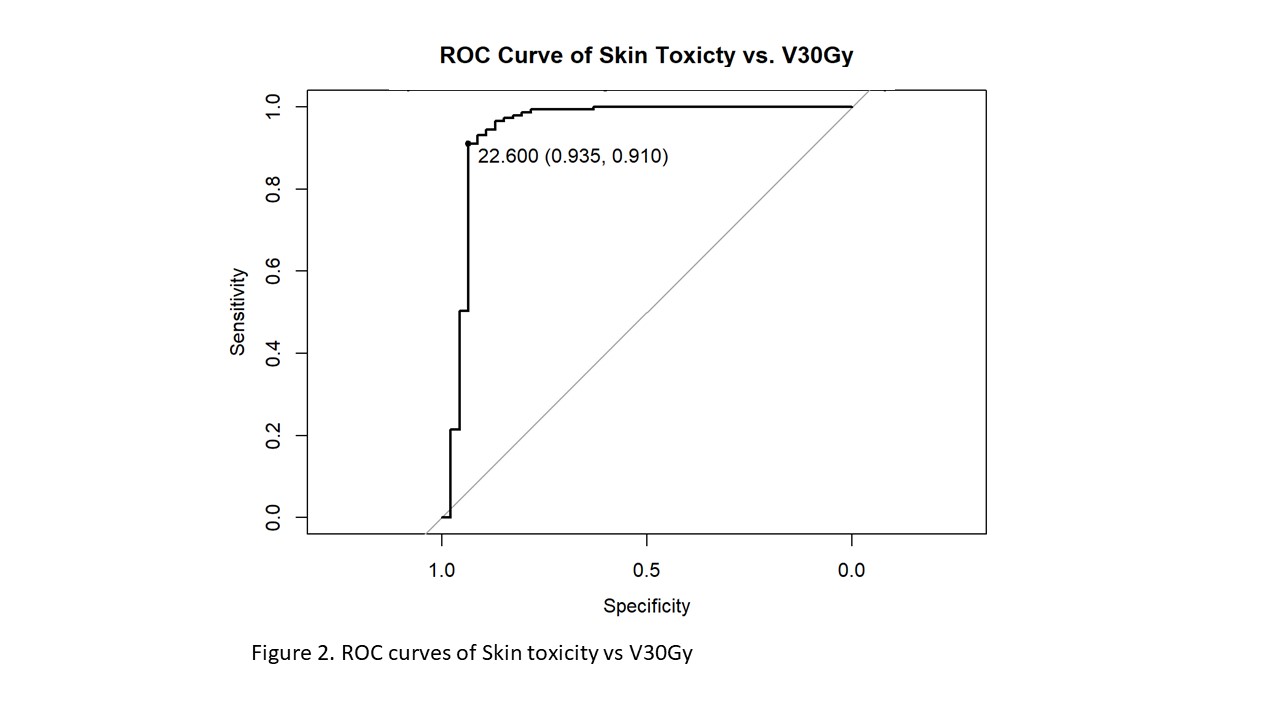
Similarly, median Dmax dose was significantly higher in the G2+ RIST group compared to G0 (60Gy vs 25Gy; P<0.0001). Using the ROC curve, we observed threshold volumes (Specificity, Sensitivity) for V10Gy, V20Gy and V30Gy to be 68.2 (0.80,0.89), 44.4 (0.89,0.87) and 22.6 (0.94,0.91) respectively, V30Gy ROC curve is shown in Figure 3. Fitting each in univariate logistic regression models, we observed patients with V10Gy > 68.2, V20Gy > 44.4 and V30Gy > 22.6 have 32, 34 and 46 more odds of G2+ RIST, compared to patients with volumes below the respective thresholds.
Conclusion
The volume of irradiated skin and Dmax are risk factors for developing acute RIST in patients treated with PBS PBT. Further analyses, including multivariable considerations, are ongoing to include a larger cohort and those with Grade 1 acute RIST to potentially identify a dose volume threshold predictive of acute RIST.