Radiotherapy in Gorlin Syndrome: Is it an absolute contraindication?
David Esteban Moreno,
Spain
PO-1407
Abstract
Radiotherapy in Gorlin Syndrome: Is it an absolute contraindication?
Authors: David Esteban Moreno1, Graciela García Álvarez2, Daniel Rivas Sánchez3, Daniela Gonsalves Pieretti4, Sofía Suarez Casanova4, Isabel Castro Rizos4, Ramón Molina Cruz4, Luis Alberto Glaría Enríquez4, Escarlata López Ramírez5
1GenesisCare Toledo, Radiation Oncology , Toledo, Spain; 2GenesisCare Madrid, San Francisco de Asis, Radiation Oncology, Madrid, Spain; 3GenesisCare Malaga, Radiation Oncology, Malaga, Spain; 4GenesisCare Toledo, Radiation Oncology, Toledo, Spain; 5GenesisCare Madrid, Arturo Soria, Radiation Oncology, Madrid, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
Medulloblastoma
is observed in 5-10% of patients with Gorling Sindrome (GS) and it usually
occurs in the first two years of life. Radiotherapy administered for
medulloblastoma in GS induces basal cell carcinomas (BCC) in the area of
radiation, so radiotherapy has traditionally been contraindicated due to reports
of BCC induction in GS.
We describe
our experience with a patient with GS treated with radiotherapy. We have also performed a
comprehensive literature review about the use of radiotherapy in BCC associated
to GS.
Material and Methods
Our case is a
73-year-old woman diagnosed with GS at the age of 33. She had multiple BCCs on
her scalp, face, head and back. Previous therapies included multiple surgeries
(Mohs last surgery on complex flap scalp), topical treatments and radiation
therapy to the back at the age of 40. The patient presented 8 new lesions on
the scalp and she refused surgery. She was treated in october of 2019 with 55 Gy in 25 fractions
with volumetric arcotherapy (VMAT) with 6MV photons over all lesions and a sequential
boost with 6MeV electrons, 10Gy in 5 fractions in two lesions greater than
3cm in diameter at diagnosis.
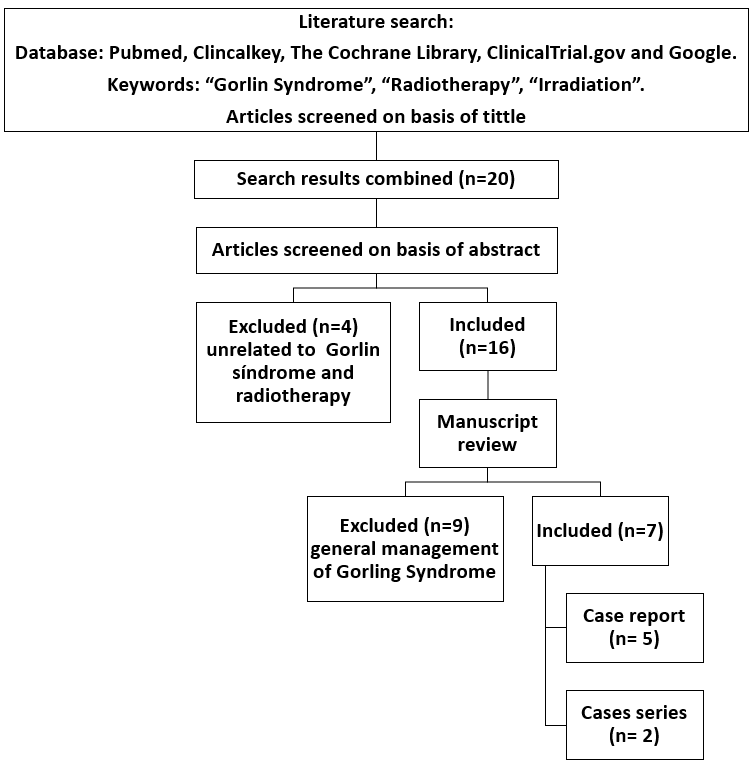
We describe the flow of information through the different phases of the literature review
in Image 1.
Results
After 10
months of follow up, our patient had fully regression of the lesions (Image 2).
After 17 months follow up, the patient presents vertigos pending study by
otorhinolaryngology without secondary malignancy tumors.
In the
literature review 5 studies show how the radiotherapy in pediatric age cause
BCC, meningiomas and mediastinal lymphoma in the area of radiation. One case
report shows an adult patient without secondary malignancy at 57 months
follow-up and made a comprehensive literature review of radiotherapy outcomes
in adult patients with GS. Another case series evaluated the use of radiotherapy in 3
adult patients with 17 BCCs treated and complete remission without carcinogenic
effects was reached in all treated lesions, with a mean follow-up of 30.35
months.

Conclusion
There is
evidence that shows how radiotherapy can induce tumors in pediatric patients,
so it is recommended to avoid the use of radiotherapy in these patient population. In
the limited literature available, there is no evidence that radiotherapy
induces tumors in adult patients with GS.
The recommend
treatment for BCCs in GS patients is surgical excision, but CO2 laser,
electrocauterization, cryotherapy and photodynamic therapy may be used. In
addition, imiquimod cream 5%, topical 5-fluorouracil and vismodegib in
locally-advanced and metastatic forms are other treatment options. However, in
selected adult patients with BCC not candidates for other treatments,
radiotherapy could also provide a favorable outcome.