Survival outcomes for p16+ oropharyngeal squamous cell carcinoma based on HPV status
Stephen Robinson,
United Kingdom
PO-1024
Abstract
Survival outcomes for p16+ oropharyngeal squamous cell carcinoma based on HPV status
Authors: Stephen Robinson1, Jonathan Towler1, Robert Kitson1, Dina Saleh1, Helen Cara Younan1, Suchana Mukhopadhyay2, Justin Weir2, Dorothy Gujral1,3
1Imperial College Healthcare Trust, Clinical Oncology, London, United Kingdom; 2Imperial College Healthcare Trust, Histopathology, London, United Kingdom; 3Imperial College, Department of Surgery and Cancer, London, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Survival outcomes for HPV+ oropharyngeal cancer are favourable, leading to calls for treatment de-escalation. Internationally, HPV status is assessed by p16 immunohistochemistry (IHC), however UK guidance recommends an additional assessment of (high-risk) HPV DNA as a second-line molecular test. However, there is a degree of discordance between methods and there is controversy as to whether p16+/HPV+ and p16+/HPV- patients have equivalent prognosis. This clouds the identification of a favourable population suitable for de-escalation. In this single-centre retrospective analysis, we compare outcomes for p16+ patients treated radically at our institution from July 2010 to July 2018.
Material and Methods
All p16+ patients were identified from our histopathology database. p16 status was assessed by IHC and HPV status (16 and 18) was assessed by DNA in situ hybridisation (DNA-ISH). Clinical demographic, tumour, treatment and survival data were collected from the electronic patient record. Differences were tested in SPSS using independent samples t-tests. Survival was taken from date of completing radiotherapy and analysed using the Kaplan-Meier method and compared using the log-rank test.
Results
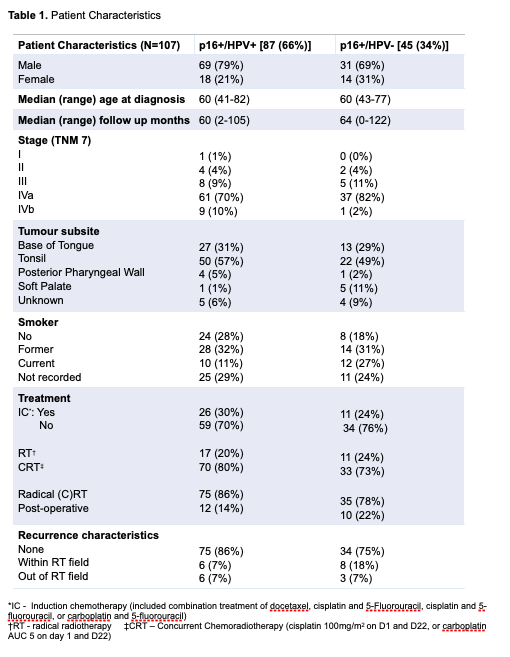
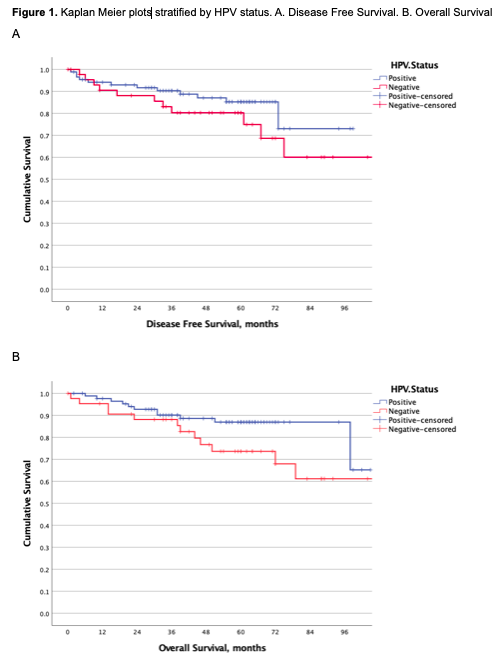
We identified 132 eligible p16+ patients; 66% were HPV+ and 34% were HPV-. Patient demographics are shown in Table 1, with no significant difference between groups. Disease free survival at 5 years was 85% for HPV+ and 80% for HPV- as shown in Figure 1A (p=0.219), whilst overall survival at 5 years was 87% and 74% respectively (p=0.103), shown in Figure 1B. Whilst the survival curves start to separate after 3 years, this was not statistically significant.
Conclusion
Our study demonstrates a much higher proportion of p16+/HPV- patients (34%) than described by other institutions (~10-20%) and no statistically significant difference in outcomes for this population. This difference in results from previous studies could be related to differences in HPV identification (DNA-ISH versus RNA-ISH versus PCR), or could have resulted from the lower number of p16+/HPV- patients included in previous analyses. The divergence after 3 years warrants further investigation by pooling data from multiple centres, but from our data p16+ patients should not be treated differently due to their HPV status.