There were 40 males and 37 females. Sixty five patients were
treated with S+RT and 12 patients were treated with RT. 38/77 patients were ≤60
and remaining 39/77 patients were >60 years age; this difference was
significant as younger patients had better overall survival (OS) (p <0.001).
In terms of T-stage, 15 patients were with T1, 25 with T2, 14 were with T3 and
23 with T4 disease. T-stage by itself
was not a significant factor (p 0.117). With regards to N-stage, 47 patients
were with N0, 10 with and N1, 18 with N2 and 2 patients were with N3 disease
and this N-stage was not prognostic factor (p 0.294). In terms of overall stage, 13 patients were
with stage I, 18 with stage II, 12 with stage III, and 34 with stage IV. Overall stage was not significant factor
either (p 0.167). Eighteen patients had
adenocarcinoma, 11 patients had squamous cell carcinoma (SCC) differentiation
with no obvious skin primary, 10 patients had other high-grade histology and
remaining 38 patients had other low-grade histology (including acinic cell,
adenoid cystic, mucoepidermoid) and this difference was statistically
significant as SCC had the worst OS (p 0.001).Six patients also had addition of concomitant
chemotherapy to the radiotherapy and this factor was not significant (p 0.676).
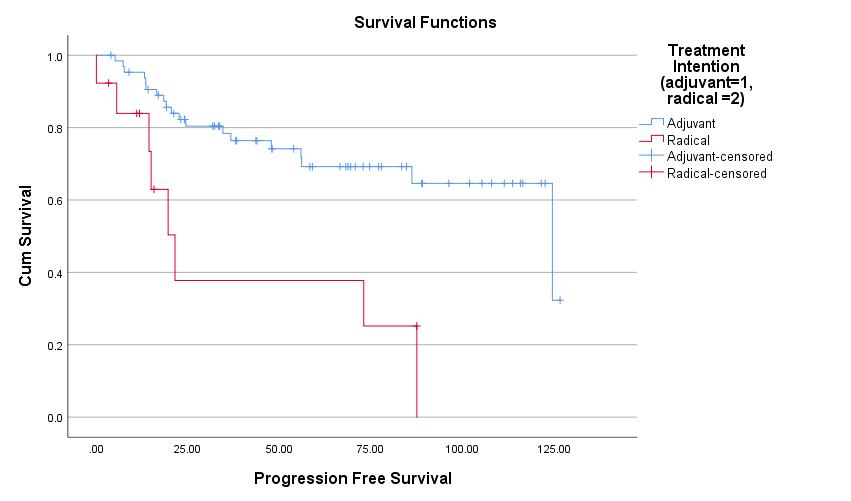
Intent of treatment was a significant prognostic factor. The mean OS was 104
months (95%CI: 89.3–119.0) for S+RT cohort versus 38 months (95%CI: 15.5-60.6) for the RT alone cohort, p<
0.0001. Estimated 5-year OS for S+RT group was 68.4% and for RT group was 28.1%
[Figure 1]. Cox regression analysis showed that S+RT group had 0.243 times less
risk of dying as compared to that of RT group (p 0.001). Even for progression
free survival (PFS), S+RT group had better PFS than RT group (mean PFS 93.38
months with SE 6.34 vs 39.93 with SE 12.0, p 0.001). Females had better
survival (p 0.001). Patients were treated with either 60-65Gy in 30 fractions
or 50-55Gy in 20 daily fractions and this dose fractionation was not a
significant factor for OS (p 0.70).
5 patients (7%) had local recurrence, 4 regional (5%) and
16 (21%) developed distant metastasis. Age (p 0.022) and N-stage (p 0.003) were
significant factors for PFS whilst gender, dose fractionation, T &
overall-stage and histology were not.