Early experience with GTV boost for prostate cancer:
comparison of MR-Linac and HDR brachytherapy
ESTRO 2024 Congress report
The use of MR-guided high dose rate (HDR) brachytherapy to provide a focal gross tumour volume (GTV) boost in the treatment of prostate cancer through radiotherapy is an established technique. However, this is resource-intense, invasive and contraindicated in some patients. Linear accelerators (linacs) with integrated MRI enable the visualisation of the GTV within the prostate, and this facilitates the use of external beam radiation therapy (EBRT) to deliver a GTV boost. This new approach is being investigated within our centre. Our studies include feasibility, dosimetry and clinical outcomes. This study compared patient-reported quality of life (QOL) for 20 patients who were treated with these two techniques.
A group of 10 patients received a GTV boost fraction using HDR brachytherapy and 10 patients were treated with EBRT through the use of a 1.5T MR-Linac. All patients received 1x15Gy to the GTV followed within a week by 5x6Gy (alternate days) to the whole prostate. Both groups received their subsequent whole gland prostate treatment on the MR-Linac. Patients reported their QOL according to the expanded prostate cancer index composite (EPIC) survey at baseline and after a one month follow-up. Additionally, details of adverse events (AEs) were collected weekly from the start of the treatment to the one-month follow-up.
Over the course of the treatment, Grade 1 genitourinary toxicity was less in the cases treated via HDR compared with EBRT (one reported AE vs. six) as seen in Figure 1, although one month after treatment, more AEs were reported for both Grades 1 and ≥2 in the HDR group than in the EBRT group (Figure 2). Mean EPIC scores were similar for bladder and bowel subscales and showed comparable QOL one month after treatment. There was a minimally important difference in the bladder bother subscale for those who received HDR, but this did not reach clinical significance. There was no mean change from EPIC baseline in either group in the rectal subscale, but a difference was seen between HDR and EBRT groups in both urinary incontinence (-5.7 vs. 1.0 respectively) and urinary irritative/obstructive subscales (-6.1 vs. -1.9).
The MR-linac focal boost to the GTV region of the prostate was found to have a favourable acute toxicity profile compared with the HDR focal boost one month after completion of the treatment, with faster recovery to baseline. This seemed to be mirrored in the QOL scores. The patients who received HDR radiotherapy were the only group to report a minimally important difference in EPIC, and this was only seen in the urinary irritative/obstructive subscale.
As this is part of an ongoing larger study, there will be longer follow-up including a larger cohort of patients, and these results may confirm whether or not these preliminary findings translate into differences in late toxicity/QOL. Analysis of factors such as organs-at-risk dosimetry, amongst others, may enable an improved understanding of their influence on toxicity and QOL. This will enable a focus on patient-centred care, in which we can offer non-invasive, outpatient-based treatment for these patients that have favourable acute toxicity rates and improved QOL.
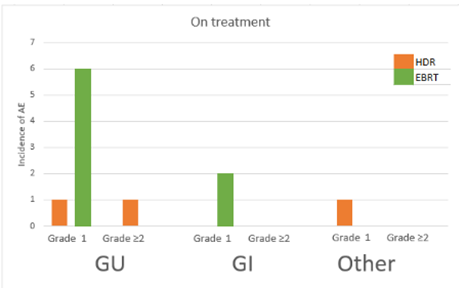
Figure 1. Incidence of AEs among patients treated with HDR or EBRT during treatment. GU: genitourinary; GI: gastrointestinal
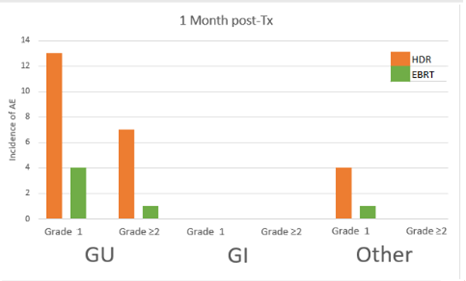
Figure 2. Incidence of AEs among patients treated with HDR or EBRT, one month after treatment. GU: genitourinary; GI: gastrointestinal
Amanda Moreira

Radiation Medicine Programme, Princess Margaret Cancer Centre, Toronto, Canada
Amanda.moreira@uhn.ca

Amanda Moreira with Michelle Leech, TipsRO Editor-in-Chief.